Going to school is a great journey with many successes and challenges for your child, family and your child’s educators. The school experience prepares your child for their growth into adulthood. These resources will help prepare your child for each stage in their education.
Starting School
Articles
- Worried About Starting School
- Getting Ready for Kindergarten
- Creating A Child Information Binder
- Facilitating Friendships between Children
- Getting ready for the first day on the school bus
- Tips for transition to school from a therapy setting for students with autism spectrum disorder
High School and Beyond
Transition Practices: Transitioning Out of High School
Ministry of education mandated items
Mary Ierullo, ASD Consultant, School Support Program, Surrey Place Centre
Transition Planning for exit out of high school
Michelle Murphy, Autism Support Teacher, Autism Programs & Services Department, TCDSB
DSO eligibility
Melanie Randall, Community Liaison Service Navigator, Development Services Ontario
Going to College
Excerpted from UN Conventions: Real Promises or Just Words
Presented by Defence for Children International – Canada and Community Living Toronto
Tuesday, May 8, 2018
Jessica Rotola and Sam Forbes talk about going to college
Person Directed Planning
With the shift from institutions to individuals, it is important to consider how to get people involved in planning for their futures and expressing what they want.
Planning for Life After School
This is a series of workshops and tipsheets designed to help plan for life after school. It is important to go through all of the workshops in order as each one prepares us for the next one.
Articles
- So your Child will be going to High School Next Year
- Tips for Transitions from Elementary School
- Transition to High School
- Transitioning to High School Toolkit
- Transition out of High School
- Looking Ahead… Together
- Transition Resources for High School, Post-secondary and Beyond
Project Inclusion
A series of five online learning modules built around lived experience stories and practical strategies intended for educators from kindergarten through grade 12. Initiated and funded by the Ontario Ministry of Education EDU, the resource is designed to help educators and school board staff combat ableism and promote accessibility, inclusion, and full participation of students with disabilities in school communities. Project Inclusion
The Benefits of Inclusion in the Classroom
Stuff to help you along the way
Understanding the Education System in the Province of Ontario

Parent’s Education Handbook
A parent handbook to help with understanding special education in Toronto and to ensure the acceptance and belonging of children with additional learning support needs. Handbook
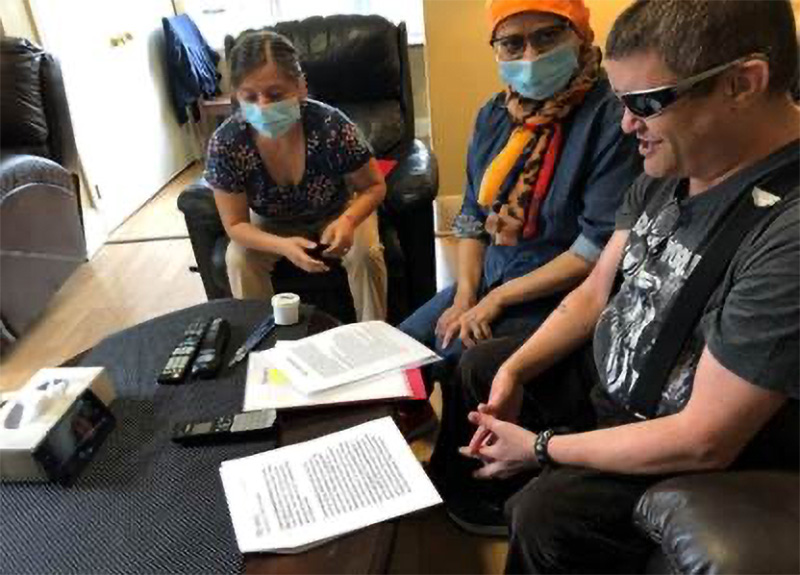
Identification Placement Review Committee (IPRC) Workshop
 Play video
Play video
In this workshop, we will take a look at the Identification Placement Review Committee the purpose of which is to discuss the exceptionality (the type of disability) and the educational placement of a student within the education system in Ontario.
Individual Education Plan (IEP) Workshop
 Play video
Play video
In this workshop we will explore the Individual Education Plan, which is a written plan of learning goals and expectations for any student in the education system in Ontario who requires modifications or accommodations to the regular school program.
A Communication Journal for Home and Classroom
For parents, teachers and caregivers, pick-up and drop-off times at the child care centre or school can be a hectic part of the day. Read more
Sharing Information with Professionals Involved with Your Child
Professionals may become involved with your child for a number of reasons. Read more
Getting The Most Out of Team Meetings
Over time, as a parent, you may come across a wide range of professionals involved with your child. Read more
Education Advocacy for Students with a Disability
This website is designed to provide an overview of the most important concepts in education advocacy in Canada. It offers knowledge and tools for families and students with a disability seeking an inclusive education, and outlines the necessary supports needed to access it. http://www.inclusionadvocacy.ca/
Disassembling Disability
Our mission is to disassemble the negativity and stigma that come when living with a disability through education and mentoring.
We offer hour long presentations on inclusivity vs accessibility as well as the history of people with disabilities. We also offer workshops on self esteem and advocacy to both elementary and high school students. https://www.disassemblingdisability.com/
Toronto agencies offering free interpretation services
A list of community organizations in Toronto that offer interpretation services. Read more
Spinclusion
A game celebrating differences and including everyone