This workshop discusses the process for registering your child for school, and easing the transition to school.
Autism Spectrum Disorder: Supporting Children and Youth – Module 5

Developing Communication Skills
Introduction
Communication is one of the core areas of difficulty for individuals with Autism Spectrum Disorder (ASD). We often think of speech as the main form of communication. Communication, however, involves much more than simply talking. A child may use words but they may not be intentional, in context, or understood by the child. A child may also be able to communicate non-verbally but not use speech.
Communication consists of verbal as well as nonverbal behaviours that take place in a social context. It includes a child’s ability to understand (receptive language) as well as to convey ideas (expressive language). A behaviour becomes communication when there is a desire to send a message to another person. The message may be sent by using words, gestures, facial expressions, tone of voice, body language, or through other means such as pictures or sign language.
Communication
Communication refers to the verbal and nonverbal behaviours that a person uses in order to convey a message to another person.
Some keys points about communication:
- It can be verbal (e.g., speaking) or nonverbal (e.g., pointing).
- It is intentional in that the person must “intend” to send the message.
- Communication is person-to-person, occurring in a social context.
The Development of Intentional Communication
Children who have not yet learned the power of communication are unaware that what they do or say has an effect on those around them. For example, a newborn baby who cries does not intend to convey a message to its mother that s/he is hungry, but cries out of distress. A mother, however, often interprets the crying as communicating hunger despite the infant’s lack of intent. It is the mother’s response to the behaviour (crying) as intentional that sets up the interaction, which is the context for the development of intentional communication. Mothers have intentional communication with their infants – they play both parts in the conversation. In typically-developing children, pre-intentional communication soon becomes intentional and by the second year most children are able to intentionally communicate.
During the first year, typically-developing infants acquire behaviours they can use to communicate their needs to others. They learn, for example, that by crying an adult will attend to him/her, that smiling and making noises gets adult attention or that an adult will say a word when they pick up an object. Regardless of the form of communication used (reaching, pointing, vocalizing), intent is demonstrated when you understand that what you say or do has an effect on someone. When a message is sent with a purpose, and with an expected outcome, the communication is intentional. Intentional communication involves the ability to persist with that behaviour until the desired effect has been reached.
Children with ASD do not develop intentional communication as quickly. Pre- and non-intentional communication may be predominant for some time even after a child has developed some speech.
Some purposes of early communication that are not intentional include:
- Practising a skill
- Reacting to an enjoyable or unpleasant experience
- Obtaining desired objects
- Soothing one’s self
Examples:
- Repeating words when no one is around
- Reaching toward a desired toy on a shelf when no one is present or looking
Reasons to Communicate
There are three main functions of communication:
- Behaviour Regulation
This is the earliest emerging function of communication. It involves requesting and protesting to satisfy immediate physical needs.
Examples:- Asking to be fed
- Trying to acquire a toy that is out of reach
- Objecting to having one’s nose wiped
- Social Interaction
Communicative behaviours that involve initiating, responding to, maintaining or ending social interactions.
Examples:- Greetings/farewells (“Hi”/”Bye”)
- Showing off
- Requesting to play games such as peek-a-boo
- Joint Attention
Communicative behaviours direct someone else’s attention to something that you are already attending to (an object, event or topic). Joint attention is critical to word learning, when labels are provided while both adult and child are focused on the same object.
Examples:- Commenting and pointing (“Look”)
- Requesting information while pointing (saying “What’s that?”)
- Providing information to someone while looking at the same item (“That’s a red truck”)
Exercise: Early versus Intentional Communication
Indicate which of the following behaviours are examples of early communication (EC) and which are intentional communication (IC).
| Behaviour | EC | IC |
|---|---|---|
| A child has difficulty opening a container of candy. S/he bites the container, throws it, begins to cry, and eventually walks away from it. His/her mother is sitting next to him/her. | ||
| A mother offers her child a glass of juice and the child shakes his/her head “No”. | ||
| A mother is talking on the phone and her child is behind her reaching for his/her train on a top shelf. | ||
| A father tries to participate with his son who is building a tower of blocks. When the father attempts to place a block on top, the child looks at him and then pushes the block away. | ||
| A child is reciting phrases from his/her favourite movie while sitting at the table. | ||
| A child walks into the kitchen and says, “Do you want a cookie?” (No one is nearby). | ||
| A child who is thirsty takes her brother by the hand and leads him to the refrigerator. |
Click here to see a sample answer
How Can Communication Occur?
There are a variety of means by which messages can be delivered. The following are some communication modes:
- Motoric
Motoric means physically moving a person/object (e.g., the child takes your hand and puts it on a toy that s/he wants you to activate.) - Gesturing
Gesturing involves moving a body part to convey a message such as pointing and/or eye gazing (e.g., pointing to milk and then looking at the adult and waiting). - Vocalizing
Vocalizing entails using sounds to communicate (e.g., the child cries to draw the adult’s attention). - Signing
Signing encompasses using either a formal or informal system of hand signs. - Using Objects
Using objects refers to passing/moving an object to communicate (e.g., passing a cup to another person to request a drink) - Pictures/Line Drawings
Picture communication includes using photos / line drawings that represent real objects (e.g., child passes a picture of a cracker to indicate that s/he would like a cracker to eat).
(Adapted from Autism: Interventions and Strategies for Success, 2001)
Communication Characteristics and Skills in ASD
There are a number of communication characteristics common to children with ASD. It is important to recognize the large range of communication skill levels among this population of children.
Communication Characteristics of Children with ASD
| Communication Characteristic | Example |
|---|---|
| Understanding / Comprehension | Inconsistent responses Over-reaction or under-reaction to environmental stimulation Literal interpretation (e.g., If told to “hop out of the car”, literally tries to hop when getting out of the car) |
| Non-verbal | Some children may not acquire verbal language Limited intentional communication Limited use of eye contact Lack of joint attention Limited gestures |
| Verbal | Reversal of pronouns (“You want a drink” instead of “I want a drink”) Echolalia *Focus of a conversation is based on own interests and fact-based |
| Written | May display hyperlexia** (precocious reading) |
| Using Language in Appropriate Contexts(Pragmatics) | Conversations and interactions lack typical “give and take” Unaware of others’ nonverbal cues (e.g., unable to judge a listener’s understanding by the expression on their face) Limited ability to take another person’s perspective Limited ability to interact or communicate with others around their interests Difficulty with understanding the appropriate distance (personal-space boundaries) and orientation relative to a communicative partner (being face to face)Limited ability to initiate, maintain and/or end conversations and social interactions Limited ability to shift topics of conversationTendency to interrupt others Difficulty providing clarifications when a person does not understand |
| Emotional | Limited display and understanding of facial expressions Mismatch between emotional expression and situation (e.g., may laugh when a person is hurt) Difficulty understanding the emotions of others |
(Adapted from The Denver Model Treatment Manual, 2001)
* Echolalia
Echolalia refers to the repetition of what another person says which includes sounds, words, and phrases. Echolalia may be immediate. This refers to when the child repeats words/phrases immediately after hearing them.
Echolalia may also be delayed. This refers to when a child hears words/phrases but may not repeat them until days/weeks/months later.
** Hyperlexia
Hyperlexia refers to an unusually well-developed early ability to decode written words, significant difficulty in understanding and using verbal language, and challenges in social interactions. This usually becomes apparent without the child having been taught explicitly to read.
Hyperlexia is a characteristic that is observed in some children with ASD, and occasionally in other conditions. This ability to remember letter patterns seems to be related to the visual learning style of children with ASD.
Variability in Communication Skills in ASD
Children with ASD vary greatly in their communication skills. Some children with ASD are non-verbal, some have limited vocabulary, and some are verbal with extensive vocabularies. Echolalia may be used by children with ASD to communicate or without purpose. As well, children may communicate for a very limited number of purposes (e.g., to request or protest), or they may communicate with many intentions (e.g., to greet, to show, to comment). Regardless of their level of communication ability, what children with ASD have in common is difficulty in communicating effectively.
How and Why a Child Communicates
In order to help a child to communicate more effectively, you must be aware of his current communication abilities.
How is the child communicating? (Mode)
- Screaming
- Throwing
- Gestures
- Facial expressions
- Looking at things
- Taking your hand and leading you
- Pointing
- Through pictures
- Making sounds
- Using words/sentences
Why is the child communicating? (Function)
- To protest
- To refuse
- To respond
- To greet
- To get someone’s attention
- To comment
- To ask questions
- To express feelings
- To pretend
Strategies to Help a Child Communicate
After observing a child with ASD and gathering information, goals can be developed and strategies selected to increase communication skills.
The following goals and strategies are categorized based on whether the child’s communication is intentional/non-intentional or verbal/non-verbal.
1. Working on Early Communication Skills with a Child with ASD
Children with ASD who are early communicators need help in understanding that their behaviour can affect another person. A goal for a child at this level might be that the child will communicate a desire for something (e.g., a toy, a drink, to go outside). If the child has some verbal language the goal might be for him/her to say the word within an appropriate context. If the child is non-verbal the goal might be for him/her to point to a picture that indicates the desired outcome or object.
Strategies to Help a Child Develop Intent
- Cause and Effect Activities
Activities that demonstrate cause and effect relationships help to develop intent. They demonstrate to the child that doing one thing causes another thing to happen. Examples of cause-effect toys are those activated by pushing a button or a switch and pop-up/wind-up toys. - Use Highly Motivating Actions and Objects
In order for a child to communicate, s/he must be motivated to do so. If a child really likes an activity such as swinging, you can start by teaching him/her to request, or make choices involving the desired activity. See Module 3 for a way to survey object and activity preferences/rewards. - Give the Child a Reason to Communicate
You can often anticipate what a child wants, especially when you know the child well. If, however, you attend to his/her need before a request, this removes the need to communicate. If you briefly delay meeting the child’s needs. s/he has a reason to communicate in order to get what s/he wants. Communicative temptations encourage a child to ask for “more”, “help”, or an activity/item by name such as “book.” For example, placing favourite items or food out of the child’s reach can encourage him/her to ask for them using whatever means that s/he can – e.g., pointing, sounds, single words, or a phrase. Reward the child by providing the item when s/he attempts to make a request or uses the means you are teaching. Always give the child time to request the activity (wait up to 10 seconds). Accept word approximations at first from non-verbal children. Reward any form of intentional communication to encourage and motivate for continued use.
Communication Skills for the Non-Verbal Child with ASD
Children with ASD may require a variety of methods both to express their thoughts and to understand what others are communicating. The term “augmentative and alternative communication” (AAC) is used to refer to alternative communication methods that can support a child’s efforts to communicate. Augmentative and alternative communication methods can be unaided or aided, using objects or devices. Examples of unaided methods of communication include gestures, facial expressions, vocalizations, and sign language (such as American Sign Language). Examples of aided forms of communication include the following: handing to an adult a cup to signal being thirsty, pointing to pictures on a communication board or in a book, and activating a device that provides auditory output.
Please note: The type of augmentative and/or alternative communication system used by a child is identified and the implementation is monitored by a registered Speech and Language Pathologist.
After determining how the child communicates (gestural, motoric, etc.), it is important to decide whether a more consistent and efficient form of communication can be used. For example, if the child often communicates by screaming or leading you by the hand, another system of communication would be more appropriate. As well, if the child does not yet speak, he needs to use another communication system, either in addition to or instead of his current means.
Below are some of the unaided ways that a nonverbal child with ASD might communicate:
- Gestures
Gestures can include pointing or looking, as well as shaking or nodding your head, pushing items away or waving “Hi/Bye.” - Facial Expression
Expressions can include requesting, protesting, declaration of feelings (e.g., happy, sad, upset, etc.) - Vocalizations
Vocalizations can include requesting for attention, refusing, affirming, greeting - Sign Language
Early signing can include requesting, protesting, refusing, greeting, etc.
The following are some of the aided ways that a nonverbal child with ASD might communicate:
- Object Manipulation
Can include reaching for items, grabbing items, handing items to adult to request, throwing items to indicate protest/refusal/dislike - Pointing to Pictures
Pointing to pictures requires the child to point to or tap the picture to communicate. The pictures may be photos, drawings, or symbols. - Picture Exchange Communication System (PECS)
PECS is a program developed by Bondy and Frost specifically to teach a child to initiate communication using visual symbols. It involves systematically teaching the child to give a visual/picture to someone to communicate, when words are not yet reliably used for this purpose. The use of PECS requires training for those who are working with the child; consultation with a Speech-Language Pathologist is recommended. - Voice Output Aids
These devices have a button that the child can activate to play a pre-recorded message. This message communicates what the child wants, or allows him to participate in an activity. For example, the child presses the button and the device says, “I want tickle”, or plays a line of a song to enable the child to “sing along.”
2. Working with a Child with ASD Who Shows Intentional Communication
Expanding the Functions of Communication
The child may be nonverbal or verbal but as long as s/he means to send messages to others, s/he is showing intentional communication. As stated above, communication takes place for a variety of reasons. Observing the child provides you with ideas as to why s/he is communicating. Your goal can then be to expand the purposes for which the child communicates. The functions of communication are as follows:
- Behaviour Regulation
Communication can be used to regulate a child’s immediate physical needs. To develop communicative behavioural regulation, you have to provide opportunities to request or protest during the daily routine. - Social Interaction
These are behaviours that initiate, respond to, maintain, or end social interactions. - Joint Attention
This communicative behaviour involves the child being able to direct the attention of another person to an object or event.
Expanding Reasons to Communicate
Expand a child’s reasons for communicating:
- Identify the best setting or time to implement the strategies (e.g., snack time, circle time, one-on-one time). This may vary depending upon the functions on which you are working. For example, greetings will be practised most naturally on arrival at the centre, or when returning to a particular room. Snack time provides many chances to practise requesting food or drink.
- Identify what you want the child to say, taking into account what is developmentally appropriate for the child and for the language used by his peers. For example, when a 4-year-old child wants a peer to join in a game, s/he may say, “Come on!” instead of “Do you want to play?”
- Encourage generalization by providing a lot of opportunities, with different people, in a variety of contexts, during the child’s daily routine.
Working with a Child who Uses Echolalia
One strategy for managing echolalia in children is to model phrases from the child’s perspective. For example, instead of saying, “Are you okay?” when the child falls down, say “I’m okay”, or “I hurt my knee”. The child will then repeat an appropriate phrase from his own perspective. If you are consistent with this, the next time the child falls down, he will have learned and may say, “I’m okay”.
Strategies to Improve Understanding
Working on the child’s receptive communication is as important as working on expressive communication. Children with ASD have difficulty processing auditory/verbal information, as well as making sense of their environment.
The following strategies can help a child’s understanding (also see Module 2):
- Predictability/Routine
Being predictable with your actions and creating predictable routines helps a child to understand what is going to happen next. This helps the child to understand what s/he is supposed to do in different situations. It also provides repeated opportunities to engage the child with language that describes what will happen in a context s/he will understand. - Using Visual Supports
Most children with ASD are primarily visual learners. The use of visual aids, therefore, enhances their understanding. Visual schedules can reduce anxiety, provide concrete reminders, and/or describe the steps in a task. - Combine Words and Gestures
Use gestures/actions when speaking to children. For example, point to a chair while asking the child to sit down, or show a picture of snack food while saying “Time for snack”. Instead of pictures, real objects can also be shown to children who need a more basic representation of the item. Written words can be shown to children who can read. - Structure the Environment
Remove or decrease distractions such as materials that are not related to your teaching/learning goals. This allows the child to better focus and to understand what is expected of him/her. Arrange the seating so that the child can better attend to the topic or task. Refer to Module 2 for other suggestions. - Simplify What You Say, Emphasize Key Words, and Repeat!
Simplifying what you say means talking at the child’s level of understanding. If the child is only able to understand short sentences, adjust what you say to match this. Try to be consistent and concise when speaking.
When you emphasize key words in a phrase, you are developing the child’s ability to understand the meaning of the request/demand/comment. Key words can be emphasized by saying them more loudly, using a different tone, pausing slightly, or making your voice more animated. To support the child’s ability to generalize the use of the word in multiple environments, use the same word for every applicable.
For example,
Doing simple imitation exercises such as waving, touching nose or ears, clapping will prompt the child to look at you and copy responses. This will also encourage the child to look at his/her communicative partner and to try different imitations such as vocalizations and gestures.
Autism Spectrum Disorder: Supporting Children and Youth – Module 4

Setting Goals and Teaching New Skills
Introduction
Children with a diagnosis of ASD have a profile of strengths and challenges. An understanding of the child’s current skills and the setting of educational goals are necessary first steps to be taken prior to addressing the building of new skills. The plan will include the prioritized skills selected for focus on and the adaptations necessary to meet the needs of the child. Breaking the learning of skills into smaller steps allows the child to achieve success while minimizing frustration. Clear and meaningful instructions will support the child’s development and ability to establish the skill.
Setting Goals
Setting Initial Priorities
When developing the educational plan, the first step is to determine the priority goals for the child. The team should be comprised of parents and educators. Avoid developing goal plans with unrealistic goals so that you and the child can see progress and experience success.
Here are some guidelines to think about when choosing a target skill to teach:
- What skills has the child achieved in each area of development? The next natural step is to build upon the existing skills in a developmentally appropriate pathway. For example, a child can sit on a trike and push him/herself forward using his/her feet on the ground. The next step would be for the educator to place the child’s feet on the pedals. The adult can support the turning motion of the child’s feet.)
- What skills would the family like the child to learn? It is very important to consider the family’s goals so that they can be incorporated into the learning environment. Working as a team will provide consistent strategies which will benefit the child. Generalization will more easily occur between settings when there is a shared approach by all team members.
- What are some everyday tasks and routines that require support?
- What skills would you like the child to learn? What do you feel is important? Is there a particular behaviour that you would like to change? For example, sitting for circle time.
- Some children have particular interests that may provide an opportunity to expand skills. Keep in mind that if the interest is restrictive and/or repetitive, you will want to expand the child’s skills to include other aspects. For example, if a child chooses to play with trains only, you may want to add people to the trains, or trains to the sensory table, or another creative activity.
- What skills can be taught at the program? Some skills may take longer to establish while others will be easily acquired.
Developing a Plan and an Outline of How the Teaching will Occur
When working toward specific goals, an educator should keep in mind the following points:
- What time of day is best for teaching a particular skill?
- What location is best for teaching?
- What modifications may be needed?
- What materials will you need for teaching (including reinforcements)?
- What kinds of group activities can be adapted to include a teaching component?
- How will you convey to the child that teaching sessions are going to happen during the week (e.g., calendar, transition cards)? Refer back to Module 2 for information that will be helpful here.
- Where will the individual support plans and other information about the teaching sessions be kept? It will be important for other staff and the child’s family to have access to this information in order to be consistent.
- With whom will you be consulting regarding the child’s learning and programming (**including outside resources, see Module 8).
Task Analysis
What is the best way to teach these new skills? While all children are unique, we know that many children need support in the following areas when learning a new skill:
- Organizing the steps
- Sequencing the steps
- Mastering the steps
- Gaining motivation to master the steps
- Generalizing the new skill to new people, places, and conditions
Organization and Sequencing through Task Analysis
It is sometimes necessary to break down a complex skill into smaller steps or actions in order to meet the learning needs of the child. The number of steps involved in a task analysis and the instructions used will depend on a child’s ability. Skills that have already been mastered do not need to be included as part of the task analysis. Provide the child with adequate time to master each step in the sequence.
For example, a task analysis for a spoon-feeding chain could be:
- pick up the spoon
- put spoon into the food in the bowl
- scoop food onto the spoon
- lift spoonful of food from the bowl
- put the food into the mouth
While the above may work for one child, another child might need much more detailed steps. For example:
- reach for the spoon
- grasp the spoon
- pick up the spoon, etc.
Once you have a task breakdown that is workable and yet flexible enough to change as you get a better sense of the child’s learning style you are almost ready to get started. First you will want to learn more about the proven teaching technique known as Chaining.
Chaining
Teaching a skill using chaining is commonly recommended if the child can only perform some of the steps, consistently skips steps, or is completing steps out of order. Backward chaining refers to teaching a skill beginning with the last step and then teaching the immediately preceding steps one at a time until the entire skill has been mastered. For example, when teaching a child a new 4-piece puzzle, leave 3 pieces intact in the puzzle and have the child place the last one. Once the child successfully places the last piece, present the puzzle with 2 pieces missing for the child to complete. Finally, provide the child with the puzzle with 3 pieces missing. Forward chaining involves teaching a skill beginning with the first step, and then teaching each successive step one at a time until the entire skill has been learned. For example, have a child place the first piece into a puzzle (with the other spaces blocked off). Once this is established, provide the puzzle with two pieces to be placed and so on.
Giving Effective Instructions
Tell me and I forget.
Show me and I remember.
Involve me and I understand.
Chinese Proverb
As educators, adults spend a great deal of time telling children what is expected of them in one-to-one teaching situations or in groups.
Giving effective instructions is an important skill to develop. It sets the stage for the child to be able to respond appropriately. Younger children with ASD, or those with limited language, often have difficulty understanding instructions which can make it harder for him/her to respond or act as expected.
What tends to happen when we give long detailed instructions is that children respond by:
- Staring
- Not attending
- Doing something else while you are talking
- Looking away
- Making sounds / vocalizing
The following are some suggestions for providing effective instructions:
- establish that the child is paying attention
- be in close proximity to the child
- give short, simple directions (e.g., “walking feet”)
- give one direction at a time
- state the direction in a positive manner
- give extra assistance if necessary and allow the child time to process the instruction
- tell, do not ask (e.g., “Time for bus” rather than “Want to get on the bus?”)
- repeat, practise and praise – make this approach a habit or routine as it will assist the child in acquiring the skill
Prompting
“Prompts” are hints or clues that can be used to help a child respond appropriately. When a child feels able to successfully complete tasks it will be more fun to practise and learn new skills.
When to Use a Prompt
Prompts can be used when the child is not able to successfully complete a task or activity independently. They are used only when needed to facilitate independence and learning.
It is helpful to use the least intrusive, most natural prompt and to fade out the prompt as soon as possible.
Types of Prompts
There are many different types of prompts to choose from, and you will likely use all of them in various teaching situations.
Prompts fall into the following categories:
- Verbal prompts – provide a verbal instruction, cue, or model of the correct response. Remember to use statements rather than questions.
Example:
“Puzzle or shape sorter” (Verbal instruction)
“Want puzzle” (Models the correct response) - Modeling – demonstrate the correct response to the child
Example:
Show how to comb your hair - Physical prompts – physically guide the child through all or part of the desired response (hand over hand)
Example:
Hold the child’s hand on the comb and help to comb his/her hair - Gestural prompts – actions such as pointing to, looking at, moving, or touching an item to indicate the correct response
Example:
Point to the circle in a group of shapes while saying “Circle” - Position cues – the correct item is placed in an advantageous position in relation to the child
Example:
Put the red square closer to the child than the blue square and say “Give me the red square”
Giving Verbal Prompts
- State the child’s name before giving the instruction.
- Give directions only when the child is paying attention. Get down to his/her level.
- Give directions slowly.
- Use directions that take no more than one or two words or simple phrases.
- Use clear and concise directions as they should direct, not distract.
- When giving directions, use words that the child understands.
- Verbal instructions may be more effective when accompanied by a gesture.
Using Modeling Effectively
Modeling will only be beneficial if the child is able to imitate.
- Model each step before asking the child to do it.
- Model bigger steps as the child gets better at imitating and remembering.
- Modeling is most effective when it is done slowly and with careful exaggeration.
Using a Physical Prompt
At the beginning of using a physical prompt, the educator is doing all the work. As the child improves, gradually reduce the physical assistance.
For example, gain eye contact with the child, let them know that you are about to hold their hand and supportively move them through the motions you are teaching. As time progresses and the child begins to understand the requirements of the task, you can move to holding the child’s hand less securely and less often. Continue to gauge the amount of support that the child requires. You may then only need to touch the child’s wrist, or forearm until the skill is established.
Determining Which Prompt to Use
Many children with ASD need a great deal of physical prompting, particularly when learning a completely new skill. Start with the least intrusive prompt and move towards more guidance as needed.
- Verbal
- Gesture
- Model
- Physical – Partial
- Physical – Hand over Hand
Start with the least intrusive prompt if you are teaching a skill the child has previously experienced and you wish to foster more independence and spontaneity.
Use a physical prompt if this is a new skill for the child, or move towards a physical prompt more quickly if s/he has had little practice with it.
Modeling and physical guidance are often the most effective prompts at the beginning, particularly for children with ASD who have difficulty with language.Accompanying a verbal instruction with a demonstration or guidance can be a very powerful teaching tool.
How Long to Use Prompts
If the child can perform a step correctly with only a verbal instruction, you are ready to move on and fade out the prompts. If not, you still need to use prompts for showing and guiding the child.
Prompts are most often associated with teaching in a one-to-one setting but they can easily be used with the child in a group setting as well. Some examples of prompting during a group setting are:
- Encouraging a child to ask another child to play by modeling “Can I play?’”
- Helping a child to participate in circle time by giving them a gentle touch on their arm accompanied by saying “Your turn.”
It is important to ensure that the child does not become dependent upon a prompt. The ultimate goal is for the child to complete this task independently without the dependency of needing a prompt. Once a child is able to complete a task independently, it will build their self-esteem and confidence to try other tasks.
Reinforcement
In a teaching situation, we want to reinforce appropriate responses in order to increase the likelihood that the child will respond again in the same way.
Used properly, reinforcers can be very powerful tools for changing behaviour.
When to Give Reinforcement
When asked to perform a task, there are four ways a child can respond:
- Attempt to escape the demand
- Avoid the demand
- Make some attempt at the task, require more support
- Obtain positive feedback for performing the task
If you reinforce the child’s attempts when introducing new skills, the attempts are associated with positive feedback which continues to motivate the child.
Reinforcers
Types of Reinforcers
- Social Reinforcers
Attention, touching, praise – this involves looking or smiling at the child, commenting on the activity the child is doing (“You’re colouring”) or (“You’re standing in line”) and give a “high five”. - Edible Reinforcers
Very small portions of food or drink. Many programs do not allow this type of reinforcer. It is typically used when a child has no known activity preferences. - Activity Reinforcers
Activities that the child likes to do are reinforcing. A successful teaching strategy is to employ the use of: “First, less preferred activity, then preferred activity.” For example, “First shoes on, then bicycle.” - Using Tokens
Tokens offer a tangible reward (e.g., stickers, stamps) every time the desired behaviour occurs. These can be exchanged later for a bigger reward (e.g., ice cream, a new book).
Key Points to Remember About Reinforcement:
- Reinforcers need to be meaningful for the child in order for them to modify behaviour. For example, if you give a child a “high five” for cleaning up but “high fives” are not that exciting to the child, this will not be motivation to maintain that cleaning up behaviour you want to see again.
- Reinforcers are most effective when they are given immediately following the desired response.
- What works one day might not be reinforcing the next day. Interests change and you need to vary your reinforcers and make them exciting.
- When you are working on a new skill, reinforce it all the time. You can start fading reinforcers (as you fade prompts) as the child gets better at the task. Reinforce only successes, then every few successes, then less often, then rarely.
Measuring Change and Keeping Records
Once you start teaching, or trying to introduce a replacement behaviour, you will want to know whether the behaviour is improving and what skills the child is learning. You will want to be able to measure the change that is happening and to keep a record of that improvement.
Describing actions with numbers (e.g., It takes Jacob 10 minutes to get in line and stand quietly.) helps you to explain how much of a challenge something is, or how much improvement has occurred (e.g., It now takes Jacob 4 minutes to get in line and stand quietly).
Remember that when trying to increase an appropriate behaviour (e.g., eye contact, interaction with other children), more time or more often is the goal. When trying to decrease an inappropriate behaviour (e.g., pinching or screaming), less time and less often is the goal.
Decide whether you want to record how often a given behaviour occurs or for how long it occurs. If the behaviour occurs a few times a day, and each occurrence is short, you may want to keep track throughout the day.
If the behaviour happens very frequently, however, or takes place over long periods, you may want to choose some specific times during the day when the behaviour is typically observed, and only record during that time.
Records of Behaviour Change (see Module 3)
There are many ways to keep records of behaviour change. You can make a graph, keep a tally of counts, keep a general communication book where you write down your observations, or keep a chart the records percentages and scores.
The important thing is that however you choose to keep track of change, you understand your system and that those who work with the child and the child’s family understand it as well. You also want to keep it in an accessible place for easy use throughout the day.
Autism Spectrum Disorder: Supporting Children and Youth – Module 3
Observing and Understanding Behaviour

Introduction
Why use observation?
All teachers need to develop skills as observers. They need to see and record as accurately and as objectively as possible what is happening in different situations. Teachers learn most about children by studying their behaviour directly. By learning to observe with objectivity, to make careful notes, and to go over the notes thoughtfully, a teacher increases his/her understanding of a child’s behaviour. Systematic observations made by sensitive and knowledgeable educators are more powerful than any other technique in determining a child’s strengths and needs. Knowing what to observe and consistently recording the information for later reference as critical to good observation. Observations can be done unobtrusively in the child’s classroom setting as s/he interacts with teachers, plays, and participates in regular transitions such as meal times. At other times, situations may have to be contrived to provide information about specific behaviours. What is being observed determines whether the observation can be natural or contrived. We observe children to determine their level of interest in, and response to. the environment, their ability to solve problems, communication skills, motor functioning, and social skills.
Observing Behaviour
Key to all observation techniques is a clear set of definitions regarding what is being observed. For example, if tantrums are to be observed, what constitutes a tantrum must be specified. What does a tantrum look like? How will you know it is occurring? Does a tantrum involve whining, turning away, crying, hitting, throwing things, refusing attempts to comfort, or some combination of all these things? Prior to the observation, the categories and their definitions must be developed, and all those using the observational instrument must be trained and skilled in its use.
There are a number of things to consider when making your observations:
- Define the specific behaviour
- Maintain objectivity and do not interpret what is happening
- Describe the behaviour you see and try not to label, (e.g., Describing a child as shy does not tell us what s/he did. We want to know that when another child approached him/her and said “hi” the child stood, looked at the floor, and said nothing).
- Determine whether the specific behaviour that you are observing requires observation in a variety of settings or a specific environment. Keep in mind that children with ASD behave differently in different environments and can be affected by other variables (e.g., visual and auditory stimuli, use of visual supports, individual, small, or large group play).
Types of Observation:
Several strategies are used to structure information gathered during observations. These may include event recording, time sampling, checklists, rating scales, and coded observations. Observations are best performed in a child’s natural setting such as their home or classroom and, if possible, by a person who is familiar with the child.
Issues and cautions to consider when using observational techniques include:
- select target behaviours
- define target behaviours in observable terms
- define the criteria to be used in judging occurrence or nonoccurrence
- select no more than two targets to observe at one time
- keep coding on data sheet simple and efficient (refer to linked documents for data collection)
- know specifically what the observation is to reveal (for example, you may have a special purpose in mind, such as trying to discover how a certain child approaches other children)
With the advancement in technology in the classroom setting, specialized equipment such as audio/video recorders may assist you in this process. It is important to be aware of your centre’s policies/procedures regarding consent of taping/recording within the classroom setting.
Event Recordings: These may be continuous, narrative records of the child’s behaviours and responses or a detailed recording of a single event. For example, behaviours such as temper tantrums may occur regularly. It is important to capture the details of the antecedent condition (what happens right before the tantrum occurs), the behaviour during the tantrum, and the consequent events (what happens immediately after the tantrum) in order to develop appropriate management and treatment plans.
Time Sampling: Often called interval recording, is used when behaviours occur more frequently and the observer is interested in the frequency of occurrence. To develop a more complete picture of a child’s behaviour you may decide to observe the child using a time sampling approach. Prior to the observation, you need to develop a form for recording observations and select the times you want to observe. Forms are usually quite simple and are typically divided into smaller intervals of 15 seconds to 1 minute. Behaviours may be preprinted on the form so that the observer can record what is occurring during each interval. The observation period may last from several minutes at different times throughout the day to an hour or more every day for several weeks. At the end of the observation period, the percentage of time that the child has spent displaying the behaviours of interest can be determined.
Checklists and Rating Scales: These can be used to determine the presence or absence of a particular skill or behaviour or to rate the quality of the behaviour or setting. Checklists of developmental milestones can be used. Children are observed at play to determine which skills they have mastered, which are emerging, and which remained to be learned.
Coded Observations: These are often used to study multiple interactions or behaviours occurring within a specified period of time. In observations of this kind, the behaviours of interest are specified prior to the observations. The number and types of behaviours can range from very few, simple behaviours to many complex interactional patterns.
How Often Are You Going to Record the Behaviour?
If a behaviour happens just a few times a day for shorter periods of time, you may wish to keep track of it throughout the day. If a behaviour happens frequently or for long periods of time, you may wish to pick specific times during the day when it typically happens. Count or time the behaviour only during these designated times. As a general rule, if the behaviour occurs more often than once in 15 minutes, you want to record only at specified times.
Understanding Why Children Behave in Particular Ways
What is behaviour?
Behaviour is anything that a person says or does. It is any action that we can SEE or HEAR. Here are some examples of behaviour:
- Smiling
- Throwing a ball
- Crying
- Scratching
- Talking
Behaviour also has a “function” or purpose. It can be a way to meet our needs, or to help us to communicate. Sometimes, when a person cannot communicate, they rely on behaviour to take the place of speaking. A child may use behaviour as a way to let you know:
- “Hey, how about some attention?”
- “It’s too loud in here.”
- “Leave me alone!”
- “I’m tired.”
What is meant by challenging behaviour?
Challenging behaviour can put the health and safety of a child, and those around him/her, at risk. It can also interfere with a child’s learning. Sometimes, behaviour is a challenge because it happens far too much, or not enough. It may take many forms, such as:
- yelling, screaming, or shouting
- hitting, kicking, or punching
- running away
- spitting or biting
- throwing things
- ignoring people, pretending not to hear them
Before one can start changing a behaviour one has to define the behaviour that needs to change. This is important, especially if you are working with a team so that everyone is looking for the same thing. For example, Sara runs from the snack table and attempts to leave the classroom. This gives everyone an understanding of the challenging behavior. Once defined, you can move into assessing the function and how to create more appropriate behaviours.
Why do children engage in challenging behaviours?
As mentioned above, all behaviour happens for a reason. It is important to better understand why a child is behaving or acting in a certain way and to determine the function or purpose of the behaviour. Simply put, what does s/he “get” for behaving in this way?
The function of behaviour can be categorized: to obtain or avoid someone or something, objects, activities; to obtain or avoid attention, or to obtain or avoid sensory stimulation. In some situations, a child might behave in a challenging way in order to make himself more comfortable. Some children can be very sensitive to the sounds, smells, sights, or textures around them. They may look for specific ways to experience sensations they enjoy, or avoid sensations they dislike. It may be more difficult to figure out behaviour that serves the purpose of trying to obtain or avoid sensory stimulation.
Examples of the four functions of behaviour:
- Access to Tangible Objects: Behaviours are used to gain access to desired objects
- Escape or Avoidance of Objects or Activities: Behaviours are used to allow a child to delay or avoid doing something that has been requested of him/her.
- Attention Seeking: Behaviours are used to gain the attention of adults or peers.
- Sensory Seeking: Behaviours are used for self-stimulatory or soothing effects.
Antecedents, Behaviour, and Consequences, or the ABCs
Understanding and changing a child’s behaviour is never simple. Describing the behaviour of concern, and gathering relevant information about when it occurs and under what conditions are the first steps to achieve success.
Antecedent is something that comes before a behaviour, and it may trigger that behaviour.
Behaviour is anything an individual does.
Consequence is something that follows the behaviour.
The ABC Functional Assessment Card is a recording system that is extremely valuable in helping to gather and analyze information to help change behaviour.
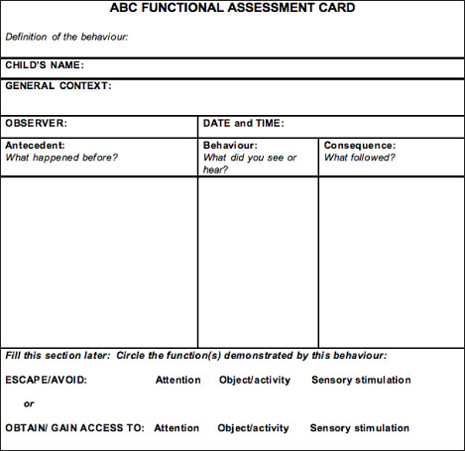
The first step is to carefully select and “define” a specific challenging behaviour. Defining a behaviour requires describing exactly what is seen and/or heard. The definition should be specific, observable, and measurable. It may be useful to print the definition of the behaviour right on the top of the ABC card.
The next step is to fill out a separate ABC Card each time the defined behaviour occurs.
Analysis of the ABCs:
It is important to look for any patterns or common trends, such as patterns in the days of the week, or times of the day when the challenging behaviour occurs. Note when the behaviour does not occur as this may give additional clues about contributing factors.
Questions to ask include:
- Is the behaviour happening during the same activity and/or with the same materials?
- Does the behaviour occur with specific people? (e.g., mom, educators)
- Are there certain events or conditions that lead up to or happen before the behaviour? These events are called triggers, or antecedents.
- Is there a consistent consequence? What happened after the child behaved in a certain way? Consequences can be positive or negative. Behaviours that are followed by a positive consequence (something the child considers pleasant, e.g., smiles, desired toys, stickers, “good job”) are more likely to recur. Negative consequences (something the child considers unpleasant, e.g., the loss of a privilege, being ignored) can decrease the probability that a behaviour will occur in the future.
- Does the behaviour stop after a particular consequence? If this is consistent, does it mean anything about the function or purpose of the behaviour?
- Consider other personal factors that may be influencing the behaviour such as illness, fatigue, or hunger.
Autism Spectrum Disorder: Supporting Children and Youth – Module 2

Setting the Stage for Learning
Introduction
Creating a successful learning environment for children with ASD may require adaptations in the following areas: physical environment, visual supports, transition strategies, schedule and routines.
Children with ASD in Group Child Care Settings
An inclusive philosophy is reflective of society’s view that all children have the right to equitable opportunities in education. While there is much variation with respect to strengths, abilities, functional levels and challenges among children, preconceptions should not be a barrier to inclusion as all children benefit from being a member of a diverse group. Inclusive settings can be beneficial for all children in the classroom.
Benefits of Inclusive Settings
- Chances to learn by interacting with other children of similar ages
- Time and support to build relationships with other children
- Chances to practise social skills in real-world situations
- Exposure to a wider variety of challenging activities
- Opportunities to learn at his/her own pace in a supportive environment
- Chances to build relationships with caring adults other than parents
- Opportunities to build friendships
Benefits of inclusive programs for typically developing children include:
- Increased appreciation and acceptance of individual differences
- Increased empathy for others
- Preparation for adult life in an inclusive society
- Opportunities to master activities by practising and teaching others
- Opportunities to build friendships
Considerations in Group Settings
Physical Environment:
Children with ASD benefit from stability and predictability within their environment. When changing or moving furniture, keep in mind that some children may need help and time to adjust to change. Changes can be made but may need to happen gradually.
Space
- To reduce running and wandering behaviours, provide smaller, more contained spaces.
- To assist children with identifying and focusing on what to do in a specific space, provide spaces that are distinct from each other for different types of play.
- To help define spaces, use shelves, furniture, and on a carpeted area, further define by placing individual mats. Create a calming corner using portable furniture for children to have quiet time.

- Reduce the amount of visually-distracting materials by keeping the classroom clutter-free.
- Keep artwork in one spot such as a bulletin board outside of the classroom rather than scattered throughout the room.
- Look for opportunities to provide natural lighting and subdued wall colours.
- Add sound-absorbing materials such as plush furniture and carpeting (where permitted).
- Have play areas that are set up for individual play, pairs, small group play, and large group play.
Materials

- Use appropriate seating which may consist of traditional chairs and tables, or more supportive seating such as a Raylax chair or Howdahug chair that promotes focus during individual or group times. Traditional chairs should allow the child to sit with good posture, have feet flat on the floor, and hips, knees and ankles at 90 degrees. Tables should allow the child to sit with elbows about 1-2” below the table top. In some cases, a chair with arms may provide additional security and boundaries for a child to help with sitting and attending.
- Promote relaxation, security, and ways to self-regulate. For example, beanbag chairs, large overstuffed pillows and child-sized rocking chairs may be placed in some spaces. A small tent with pillows inside and heavy quilts on top may offer an opportunity for brief respite from noise or others’ activity. Sensory materials such as rice bins, playdough, and tactile boards can be calming for some children.
- Provide for physical activity using heavy objects to lift, carry, or push. Schedule use of these materials regularly and between activities that require focused attention as a way to regulate emotions and prevent disruptive behaviours before they happen..
Visual Supports
Adults rely on visual helpers every day such as calendars, day timers, street signs, grocery lists, maps, and so on. Visual cues in the environment allow planning, organizing, and independence. Visuals are equally important to children because they are just beginning to learn how things work in the world.
Why do visual supports make it easier for children to understand and communicate?
- Words “disappear” right after we say them but visuals hold time and space.
- Visuals direct attention and hold attention.
- Visuals allow more time to process the information.
- Visuals assist in remembering.
- Using the same words every time a visual is shown teaches the child those words.
Anything we see that helps us with communication by giving us information for our eyes is a visual support. The type of visual that works best with each individual child depends on what is meaningful to the child. The most widely-recommended visuals are those that are used to provide children with information.
For example, labels placed around the home or classroom help to inform the child where to find and where to put materials. Rules provide your child with clear expectations. Other types of visuals that give information in a logical, structured and sequential form consist of schedules, mini-schedules, and “first/then” boards. Activity choice boards allow the child to make selections during their play.

The previously named visuals can be presented in several formats, depending on the child’s level of understanding. Ranging from most concrete to most abstract, possible visuals are:
- Objects – would be considered to be the first level of visual representations and would include the actual objects (e.g., for some children, seeing a sandwich in their parent’s/teacher’s hand tells them “It’s time for lunch.”)
- Colour photographs – would consist of coloured photographs of concrete objects (e.g., for some children being shown a photograph of a bus means “We’re going to daycare” or “We’re going home.”)
- lack and white photographs – would consist of the same photographs but in black and white
- Colour line drawings – picture symbols that are often used with children who are able to understand at this level of abstraction
- Black and white line drawings – also picture symbols and serve the same purpose as coloured line drawings
- Miniature objects – smaller versions of the objects
Tip: Remember to place visuals at the child’s eye level.
Preparing for Transitions
For many children, routines and structure are important because they provide a sense of security. Even slight changes in the usual routine can be highly upsetting. Preparing for transitions and having consistent routines help children to cope with change.
Children may have difficulty making transitions for many reasons. Here are some examples:
- Change is unexpected For example, weather prevents children from going out for regularly scheduled outdoor play.
- Current activity is enjoyable For example, child does not want to stop present activity for another event.
- Dislike or fear of the next activity For example, child knows what the next activity is and does not like it or is afraid of it, so resists getting ready.
- Next activity is enjoyable For example, child leaves present activity early in attempt to start enjoyable activity before it is time.
There are two main types of transitions:
- Daily: Major transitions during the day for young children usually involve sleep, mealtimes, or changes in the environment/location such as:
- From one activity to another
- Indoor to outdoor play
- School to home
- Life These are transitions that occur once in a while (e.g., starting a new job, having a baby, or moving). Children need extra care and attention during these times because change can be upsetting and frightening to them. For example, at daycare a child may be moving into another classroom with a new teacher and new children or a child may be moving to a different house.
Strategies to help a child make transitions:
Provide verbal warnings
Use warnings that a transition is about to occur. For example, “It is almost time for lunch.” The transition can be made concrete by setting a timer or counting down from ten after giving the warning.

Fidget Toys
If a child is finished with an activity but needs to wait for another one to begin, playing with a fidget toy (e.g., squishy ball) can help him/her keep busy. Experiment with a variety of fidget toys and choose ones that do not make noise and that the child is able to keep in his/her hands or pocket.
Transition Objects
Try using an object to signal that a new activity is about to begin. For example, if the child is playing and it is almost outdoor play time, bring the jackets into the room within sight.
Music
Songs are a fun way to signal that the current activity is about to end and a new one will be beginning. They help children learn routines and improve language and memory skills. Try using the same tune and changing the words for different activities. This will make it easier for children to remember the song and join in the singing. Learn more about transition songs by visiting the Creative Circle Time: Music, Stories and Games Workshop.
Visual Cue
To gain children’s attention, turn the lights off and on or say, “Put your hands on your head.” Once you have the children’s attention, begin the transition by singing, “It’s time to tidy up. Tidy up. It’s time to tidy up!” The song could be followed by two handclaps before turning the lights back on and then the children start to tidy up. This combination of strategies works because gestures and songs catch children’s attention.
Visual Schedule
Using objects, photos, or pictures to show a child the order of activities that are planned can help him/her understand what is going to happen next. Here is an example of a visual activity schedule.
Create visual schedules using photographs, pictures from magazines, or the Visuals Engine on this site. When first using a visual schedule, include one or two transitions. Gradually add more, up to a maximum of six or seven pictures in one schedule, based on the child’s developmental level.
To help a child understand when an activity is finished, attach pictures to a piece of bristol board using tape or velcro. As each activity is finished, a child can remove it from the schedule and put it in a small box or envelope labeled “finished”.
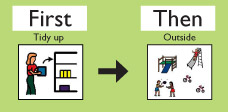
For some children you may want to have a full visual schedule of the day on the wall for reference. For transitions you might want to have a separate one that shows what is ending and what is starting. For example, “First tidy up then go outside”. Using a “first/then” visual to break down the immediate expectation can help the child understand what is coming next. This can also help the child to focus on the transition and what he/she needs to do.
Schedule and Routine
Schedules, predictability, and routine are essential for a child with ASD to function well, particularly in a group setting. Keep in mind the following:
- Provide consistent and frequent use of visual schedules of the daily routines and activities.
- Maintain a routine that does not vary much from day to day, especially when a child is new to the program.
- Ensure that the location of materials and equipment is consistent.
- Maintain an initial consistency in the staff the child will encounter daily to help establish routine.
- As the child becomes more comfortable, introduce small changes gradually to help him/her develop some flexibility. Examples could be changes in routine, place, and staff, using visual supports and schedules to cue the changes to the child.
- Provide a written individual schedule for the child with ASD, showing what s/he will be doing and with whom. Post this where it can easily be seen by staff to maintain consistency and structure for the child.
- Provide consistency for staff as well. Provide a written schedule of who will be where, doing what.
- Schedule routine time for staff to plan and communicate about the needs of a child with ASD, with parents and consultants as needed or available (see Module 8).
Autism Spectrum Disorder: Supporting Children and Youth – Module 6

Developing Functional Play and Adaptive Behaviour
Introduction
Children with Autism Spectrum Disorder often have challenges with functional play skills and adaptive behaviour (tasks associated with daily living). They benefit from environmental supports and direct instruction to develop their play skills and independent living skills. There are strategies and supports that incorporate direct teaching of play and other adaptive skills to develop essential skills. See Modules 3 and 4.
Developing Functional Play
1. Definition and Importance of Functional Play
Functional play can be defined as play with toys or objects according to their intended function (e.g., rolling a ball, pushing a car on the floor, pretend feeding a doll).
Play is a way children learn to make sense of the world. Functional play is a powerful tool for developing cognitive and social skills. Play develops a child’s problem-solving skills through the discovery of properties of actions and objects (e.g., hard/soft, fast/slow, and how things work together).
Functional play is also important in social interactions. Children interact with each other through play with toys, equipment, and action sequences. Sharing enjoyment in play develops a sense of connectedness with others.
2. How Children with ASD Play
Children with ASD may exhibit a range of play behaviours. The range of the play behaviours is dependent on the child’s level of development and the accessibility of supports and structure in his/her environment. From earlier to later developmental levels, these behaviours can range from:
- Appearing uninterested in objects, toys and peers
- Repeating actions with objects (e.g., spinning the wheels of a toy car, or lining up blocks).
- Limiting play sequences: only appropriate single actions with toys (e.g., shaking a maraca,pushing a car on the floor, or swinging on playground equipment).
- Creating more elaborate play sequences involving two or more actions with toys (e.g., putting a ball in a hole, hammering, building a block tower then crashing into it with a car, stringing beads, using a marker on paper, feeding a baby doll with a spoon).
- Linking related play sequences (e.g., putting the doll to bed, waking it up, feeding it).
- Displaying organized play (e.g., initiating play with an object, using it appropriately, putting it away and finding another object).
3. Why Play is Difficult for Children with ASD
This is not well understood. The possible reasons include difficulty with:
- Attending to functional play aspects of the toy or object
- Adjusting to novel or sensory qualities (e.g., noisy toys or those with certain tactile qualities)
- Imitating the actions of others
- Generating novel ideas about how to play
- Knowing how to initiate, sustain, and end a play activity (changing with the natural flow of play)
- Understanding how to share the enjoyment of play with others
4. Supports for Play Needed for the Child with ASD
Almost all children with ASD need support to develop their play skills. These supports might include:
- Setting up the environment so that the child is able to focus (see Module 2)
- Engaging the child in what interests him/her and can be jointly enjoyed
- Gradually introducing new toys and sensory experiences because some children need to be exposed to a new toy for a while before initiating a purposeful interaction
- Task analysis -Breaking play down into steps (see Module 4)
- Modeling how to play with the toy
- Guiding the child to play with a toy or piece of equipment and gradually fading support
- Encouraging the child to imitate his/her peers
- Providing visual supports so the child can be a more independent player (choice boards or mini schedules (see Module 2)
- Providing rewards or favourite play activities alternated with successful play attempts
- Creating desirable opportunities for the child to learn
- Generalizing play sequences into a social context (e.g., a teacher facilitating a game with a child and his/her peers)
Always provide positive feedback and reinforcement for appropriate play. If this is a new skill the child is learning, s/he will need more validation and higher praise at first. Remember, to see a behaviour or a skill again the child must be validated and reinforced.
Adapted from the Denver Model Treatment Manual, 2001
Teaching Adaptive Behaviours
1. Definition of Adaptive Behaviours
Adaptive behaviours are skills that support basic daily living functions (e.g., using a fork, putting on boots, blowing your nose).
Adaptive behaviours are usually sequences of movements put together to achieve a specific outcome (e.g., eating, dressing, toileting, hygiene activities, chores, and sleeping). These skills usually occur in the context of daily routines, in a particular place, and at a particular time each day.
Adapted from Steps to Independence, 1997
2. Difficulties with Adaptive Behaviours
Delays in learning adaptive behaviours can be caused by difficulties with:
- Initiating and continuing a sequence of movements (motor-planning challenges)
- Heightened awareness of sensory qualities (e.g., textures/tastes of food; feeling of clothing; sound /feeling of hair-cuts or shampoos)
- Focusing on a task
- Gross and Fine-motor skills
- Cognitive delays
3. How to Work with Adaptive Behaviours
The principles of OBSERVE, THINK, TRY are recommended.
Find a way to measure and record how the child is progressing. It is a good idea to keep the chart simple and handy.
The chart could be kept near where the skill is being taught so that staff can easily check off (e.g., on a clip board high on wall by the snack table with a pencil on string taped to it). (See Module 4, for more examples of charting).
Set up a way to communicate with other staff and the parents. Ongoing communication between the team members is imperative in successful teaching. Talk to staff and parents about strategies used, or create a communication binder or notebook to travel with the family. Implement the plan and record progress. Evaluate progress and alter the plan as needed. The child may not demonstrate signs of change immediately, so it is important to remain consistent with the plan for at least two weeks. The plan may need to be modified depending on the child’s progress within a reasonable amount of time. Set new objectives on a regular basis, or at least every 3 months.
4. Teaching Adaptive Behaviours
In order to help a child experience success, she/he must be provided with the right level of support and rewards. As the child progresses, the frequency of support/prompts and rewards can be gradually decreased. This helps the child to succeed by working in small steps towards the desired skill.
Consider the learning style of a child with ASD.
- May find it challenging to follow verbal directions and imitate
- Usually responds well to visual supports and physical guidance
Ways to help a child learn an adaptive behaviour skill:
- Teach within the natural routines when the skill is needed
- Teach the child to use cues from the environment (e.g., initial brief verbal instruction to get dressed, the sight of clothes in the cubby, a picture schedule)
- Reduce verbal cues (reduces reliance on adult presence)
For some children, modelling the task will be enough to help the child learn the task. For many children with ASD, once the initial direction has been given and a model has been shown, the child may require guidance to ensure success.
Sometimes it can be most effective to give and fade support throughout all the steps of a task. This “whole task” approach means that the child does the parts they can in the sequence and is prompted for the other steps.
In other situations, it may be best to focus on helping the child complete only the first step or the last step of the skill. From there, you can build on this initial success by focusing on the next step until the task is complete. These approaches are called, respectively, “forward chaining” and “backward chaining”. An example of backward chaining is as follows: first help Billy to put on his sock until the final step of pulling it up past his ankle. Next time, assist until the sock is barely over his heel, and let him complete the two final steps, pulling up the sock over the heel and past the ankle. In this approach, you are setting up the child for success. Remember to heavily praise the child for completing the task. This will motivate him/her to continue practising the new skill as the task gets more challenging.
If the child can match pictures to objects, you can make a picture schedule of some of the steps involved in certain skills (seen in Module 4). Place the picture schedule where the task normally takes place. Guide the child (as needed) to point to each picture to help complete the steps. Then guide him/her to do the step indicated. As the child progresses and moves through the steps independently, remove the steps s/he has mastered from the chart.
Keep the chart as long as the child needs support to go from one step to the other (e.g., a Velcro strip near the child’s cubby may have pictures of clothing items in the sequence. Guide the child to point to first picture, find the item, put it on, then turn over the card, and point to the next card, find the item, put it on, etc).
Try to provide a natural consequence as a reward for completing the skill (e.g., being able to go outside after getting dressed or drinking juice after fetching and pouring it).
Many repetitions may be needed to gain independence. The child receives support to complete what he can on his own. This gives the child a sense of mastery and reduces frustration.
5. Problem Solving
What About the Child Who Does Not Like to be Touched or Guided?
Children who do not like to be touched should be approached more slowly and gradually. Look for types of touch that the child does tolerate. Often firm, broad touch is more acceptable than lighter or more tentative touch, and it can help to relax a child. Some children prefer to be touched on the feet or back. Look for pleasurable ways and times in the day to provide touch experiences so that the child gradually accepts being touched. A good way to do that is through “sensory social routines” such as familiar songs and games that incorporate pleasurable touch experiences. These can be done at the beginning, end, and at various times throughout any activity.
Review
- Children with ASD often have delayed play skills.
- They benefit from direct teaching of play skills and additional supports for independent play.
- Children with ASD may have delays in learning adaptive behaviours or the skills of daily living.
- Adaptive behaviours can be supported and taught in a systematic way within the daily routines in which they occur, as well as in specific teaching sessions.
Autism Spectrum Disorder: Supporting Children and Youth – Module 7

Enhancing Social Skills
Introduction
Children with Autism Spectrum Disorder (ASD) experience challenges in social relationships. A deficit in social interactions and communication is one of the identifying characteristics of ASD. Children with ASD may appear uninterested in social interactions and may have difficulty understanding the behaviour of others. Children with ASD may desire social engagements but lack the necessary social skills to develop these relationships.
What are Social Skills?
Social skills are the verbal and nonverbal behaviours that allow people to participate in various social situations.
1. Why Teach Social Skills?
We understand that children with ASD learn new skills differently (see Module 4). In the same way, social skills must be explicitly taught. Children with ASD take in information about the world and respond to that information in a different way. This has a profound effect on their ability to interact with people.
Social and communication skills are highly interdependent. Difficulties in both of these areas have separate and joint effects on an individual’s ability to develop and maintain relationships with others. Children with ASD may experience a lot of confusion and frustration as a result of these difficulties. This can lead to secondary problems such as tantrums, or other challenging behaviours. Promoting social and communication skills can be critical in the overall well-being of a child with ASD.
2. Social Development Milestones
Typically-developing children show the following social behaviours by approximately the ages indicated in brackets:
- Smiles at familiar adults (1½ months)
- Imitates simple actions (9 months)
- Engages in a simple game with others, such as rolling a ball back and forth (1 year)
- Imitates actions of another child (1½ years)
- Watches other children play and attempts to join briefly (2 years)
- Plays alone, in presence of other children (2 years)
- Plays simple group games (e.g., Ring Around the Rosy) (2 years)
- Begins to take turns (3 years)
- Forms temporary attachment to one playmate (3½ years)
- Takes turns and shares without supervision (4½ years)
- Plays cooperatively with up to two children for at least 15 minutes (5 years)
- Has several friends, but one special friend (5 years)
- Plays cooperatively in large group games (5½ years)
(Adapted from A Work in Progress, 1999)
Social Skills of Children with ASD
The social skills of children with ASD may differ from those of typically-developing children (see Module 1).
Below are some characteristics of social skills that children with ASD may demonstrate:
- Often shows attachment to familiar adults, such as a parent, but may be uninterested in other adults and children
- May demonstrate an awareness or interest in others but may not have the social skills to interact appropriately
- May have difficulty imitating peers
- Imagination and pretend play are limited and play is generally repetitive
Identifying Social Skills
1. Social Skills to Target for Young Children with ASD
(Note: overlap with early communicator skill targets)
- Attending to objects
- Being with other children
- Imitating
- Sharing
- Turn-taking
- Asking for help
- Using social conventions (e.g., “Please”, “Excuse me”)
- Voicing greetings and farewells
2. More Advanced Social Skills to Target for Children with ASD
- Displaying peer entry skills
- Offering help
- Asking someone to play
- Playing a game
- Identifying emotions and other nonverbal cues
Self-calming techniques and social skills
Self-regulation may be essential for promoting appropriate peer interactions, although it is not considered to be a “social” skill. The child’s ability to manage his own body, mind, and emotions make successful inclusion with peers more likely. These particular adaptive skills may at first require a great deal of adult support. See Module 2 for adaptations to the environment that assist children in coping with a group setting. See Modules 3, 4, and 6 for strategies to teach adaptive “self-calming” behaviours.
Social Skills
It is important to observe both the child and the child’s peers in order to ensure that the social skills activities are as follows:
- Consistent with the child’s likes/dislikes
- Lending themselves to interaction with others
- Age appropriate
- Peer appropriate
NOTE: Although making activities age and peer appropriate is the goal, the child’s skill level and interests must also be taken into account.
Toys, games, and ideas to encourage social interactions:
- “See & Say”
- Simple foamboards/ puzzles
- Dolls, stuffed animals
- Shape sorter
- Swings
- Cars, vehicles
- Musical videos
- Music
- Peek-a-Boo
- Action songs
- Colouring
- Activity Centre
- Solitary play
- Ball
- Tea Party/ Birthday Party
- Chase
- Ring-Around-the-Rosy
- Lego, Blocks
- Cars, Vehicles
- Marble maze
- Puzzles
- Dolls, action figures
- Painting
- Play kitchen
- “Candy Land”
- Matching games
- “Snakes & Ladders”
- T-Ball
- Soccer
- Construction play
- Pretend play
- Socio-dramatic play
Adapted from A Work in Progress, 1999
1. Strategies for Teaching Social Skills
Joining In
Children with ASD may have challenges initiating and including others in their play. Start with games that do not require toys, such as physical activities like tickling or chase. Structured activities are predictable and become routine. They will eventually leave little to interpret and can be easily taught. Games with repetitive actions, sounds, words, and movements/sensations that the child enjoys encourage social interaction. Singing games like “Ring-Around-the-Rosy” or “Row, row, row your boat” encourage simple social engagement and turn taking.
During “Row, row, row your boat”, pause and allow the child to take a turn by filling in a word and/or the action. Then take your turn and keep the song going. Provide prompts when necessary for the child to take a turn at first. The more practice a child has had with joining activities with another person, the more successful s/he will be when playing with other children.
Tasks that highlight a child’s strengths and interests may be used in peer-directed activities. For example, a child with an interest in weather might take charge of posting the day’s weather on the calendar during circle time.
Play with Peers
Promote play with other children by choosing activities that are predictable, structured, and of interest to everyone involved. Consider games the child with ASD already knows and has played independently. Determine distinct roles to encourage cooperative play, sharing, and turn taking. Adult prompts and modelling may be required to initiate and sustain play interactions among peers. It is important to remember that the goal is to teach the child with ASD how to play with his/her peers.
Here are some toys and combinations that provide opportunities for cooperative play at various levels:
- Ball or car: “sender” and “receiver” (on floor, down a slide)
- Bubbles: “blower” and “popper”
- Toys in the sandbox: “hider” and “seeker”
- Containers, various materials: “filler” and “dumper”
- Talk about a pre-selected topic of interest: “asker” and “teller”
- Cooperative building (Lego, blocks): “builder” and “knocker down”, “block chooser” and “builder”, or take turns placing blocks
- Wagon: “rider” and “puller”
(Adapted from: Social Skills for Young Children, IWK Health Centre; and A Work in Progress, 1999)
Exercise: Developing Play with Peer
Choose a cooperative peer and ask them whether they would like to play a game with ___________ (the child with ASD). If the peer agrees, arrange a brief game during which you may provide the children with prompts when necessary to ensure some success for the child with ASD (e.g., popping the bubbles, completing the puzzle, knocking down the tower of blocks). Be sure to build in positives for the peer partner (e.g., praise, access to another preferred activity after the game).
Click here to see a sample answer
Visual Supports
Visual strategies have been identified as effective supports for children with ASD in their communication and cognitive development (Modules 2 and 5). They can also help children with ASD develop social skills. Visual aids act as a reminder and breakdown the expected tasks involved in appropriate behaviour in social routines.
- Cue Cards
Cue cards are visual aids that remind the child what to do in social situations. They are pictures or symbols used to replace or reinforce verbal directions, or used to quickly and quietly redirect a child. Cue cards can be used to prompt appropriate social scripts, such as “It’s my turn,” or “Hi”. Cue cards also promote appropriate behaviour like “Line up” or “Hands to self”. For cue cards to be effective, consider the child’s strengths and abilities. - Social Scripts
Social scripts are visual aids used to demonstrate language to the child with ASD in social interactions. They are arranged to depict appropriate behaviour in a social situation. Scripts typically involve a series of visual cues. For example, a script for greeting someone on arrival at preschool could be three visuals depicting: (1) Open door; (2) Say “Hi” to____; (3) Stop (wait for ____to say “Hi”).
The picture sequence should be placed next to the door or given to the child by the parent to view before entering the room.
Visual scripts can also be used to guide a child through a play activity with another person. For example, to help a child to participate in a bubble-blowing activity, a visual script could be used to cue the child to: (1) wait for the other child to blow bubbles; (2) pop the bubbles; (3) say “My turn”; (4) put out a hand for the container of the bubble solution.
Note: The pictures in a visual script should be aligned and read in a row; either horizontal (left to right) or vertical (top to bottom) depending on what the child is used to. - Social Stories
A social story is a short story that describes a situation, concept, or social skill. It includes information about what to expect in the situation and why. These stories may improve the social understanding for children with ASD. Social stories can be written to address any number of topics, including self-help skills, social interactions, changes in routine/environment, and behavioural strategies. Social stories are written in the first or third person to provide a literal and concrete understanding of appropriate behaviour. Carol Gray’s The New Social Story Book – Illustrated Edition provides guidelines for social stories.
An example of a social story for a simple behaviour is as follows:
Review
The following are key points to remember:
- Social skills are significantly impaired in children with ASD.
- This impairment compounds difficulties in other areas, such as communication and behaviour.
- Social skill targets have to be chosen carefully based on criteria such as age and interests.
- The use of games, visuals and social stories are three of the strategies that can be used to help a child to develop appropriate social skills.
- Plan activities that naturally bring children together.
- Facilitate interaction with peers by providing the child with peer-directed tasks, and give prompts as needed.
- Efforts should be made to generalize social interactions across different settings and people.
Autism Spectrum Disorder: Supporting Children and Youth – Module 8

Working Together
Introduction
The complexity of the needs of children with Autism Spectrum Disorder requires the integrated efforts of a community. This includes family, educators, health care providers, and others. It is important to facilitate collaboration among the child’s family and professionals in order to work towards established goals to best support the child and his/her family.
Who are the Team Members?
Most children are born into families with community support. When a child has extra support needs they become part of a larger community. This community may include different professionals and services such as child care centres, early intervention programs, health care services (e.g., speech-language pathologists, psychologists, physiotherapists, physicians, occupational therapists, nurses), community services (e.g., social workers), and recreational programs. Each part of the community plays a specific role and brings a different expertise to developing a good, integrated program.
Parents are the experts and guardians of their child. They live with the child and know his/her likes, dislikes, tendencies, and personality. The family’s input is essential in the development of goals for a child’s program.
A few principles to guide interactions with parents and family members:
- Treat the parents’ views with respect. It is important to ensure that the relationship between families and professionals is collaborative and respectful.
- Maintain an objective perspective. Every family is unique and there may be many factors involved when making decisions. Treat the family as a unit, focusing on balancing the needs of all members involved, including siblings.
- Keep in mind that being a parent of a child with ASD brings new stresses to a family’s daily life.
- Professionals are guides, not experts
- Collaborative relationships involve a cooperative approach to problem solving and support. They require openness and sharing.
- Ultimately, the family will maintain responsibility for decisions involving the child with ASD. Professionals must realize that their involvement typically constitutes only a fragment of the total picture for the child and family
- Our goal is to create a partnership with the parents while working with the child. Creating shared goals for the child and respecting what every professional and parent/family member brings to the table helps the child to reach those goals.
Modified from Working with Families: A Developmental Perspective, 1987.
Team Members:
Family
Family members will typically have detailed knowledge about the child’s daily life. It may be helpful to obtain information about:
- Play activities the child enjoys
- How the child communicates at home
- How you can communicate best with the child
- Activities the child does not enjoy
- Strategies that help the child to calm down
- Rewards or reinforcers that motivate the child to learn a new skill
- Times of the day the child prefers to rest and relax and times the child prefers to be active
- The child’s preferences related to the following: positioning, diet, temperature, lighting, and sound level
- Special needs related to health and development such as toileting, dressing, and grooming
It would be beneficial to maintain ongoing communication with the family about their hopes and dreams for their child and anything that may be of concern. Families are a great source of information and resources about ASD to be shared with other team members.
Clinical Psychologist
A clinical psychologist has in-depth graduate training in learning and behaviour. S/he has the necessary training to administer and interpret formal psychological tests, diagnose, and provide intervention services for individuals with ASD. Psychologists examine children’s verbal and nonverbal cognitive skills and adaptive behaviours (e.g., self-care, social, motor, play). With training in behavioural-intervention methods, they can assist in developing and teaching programs for children with ASD. They are also equipped with professional skills to provide families with coping strategies to get through stressful circumstances.
Early Interventionist
Early interventionists are trained and experienced in working with families and children with special needs. They come from a variety of backgrounds, including special education, psychology, and early childhood education. They help families identify goals and organize resources. Activities are designed by early interventionists to complement the family and the child’s routine.
Occupational Therapist
Occupational therapists focus on functional and developmental needs. They examine a child’s fine motor skills, sensory processing, visual perception, organizational difficulties, oral/motor development, and seating/mobility needs. They pay particular attention to motor planning abilities related to the development of self-care, play, and social interaction skills.
Physician
Several different types of physicians may be involved in a child’s care, depending on his/her individual needs. The family physician makes referrals to specialists such as pediatricians, developmental pediatricians, neurologists, and psychiatrists. A pediatrician has special training in children’s health needs. Pediatric neurologists, developmental pediatricians, and child and adolescent psychiatrists have additional training and experience in diagnosing and managing certain aspects of child development and behaviour. Physicians are responsible for the management of medication. Neurologists typically also become involved when a child has a seizure disorder. In different centres, one or more of these specialists may be involved in the care of children with ASD.
Social Worker
Social workers have specialized training in family functioning. They gather information about the family history, relationships, and supports. They also provide support for the management of family stress and communication. Social workers typically have a good appreciation and awareness of community supports. They are strong advocates for families to access additional financial and recreational help, respite care, and social support.
Speech-Language Pathologist
Speech-language pathologists observe, evaluate and develop interventions to promote children’s communication skills. They will examine the child’s ability to understand communication (receptive language), ability to communicate with others (expressive language), social use of language (pragmatics), ability to control their tongue, lips and jaw (oral-motor functioning), ability to produce speech sounds (phonology/articulation), pitch, loudness, resonance (voice), and smoothness of speech (fluency). The speech-language pathologist may also assess and develop interventions to promote social interaction and play skills.
Other Professionals
Many other professionals may be involved, depending on the child’s needs. Physiotherapists provide support for the development of gross motor, mobility, and play skills. Nutritionists provide counselling and support regarding the dietary challenges that are common in children with ASD. Audiologists assess hearing and ophthalmologists assess vision. Geneticists are often involved when examining possible causal factors in the child’s disorder, as well as when families are considering having more children.
In the wider community, children with ASD and their families may also benefit from extended family, informal or formal support groups (e.g., autism societies, Association for Community Living), spiritual counselling or membership in a religious community, recreational programs (inclusive or specialized), opportunities to access respite care providers, and a variety of other supports. Each family will differ in how they define the team of essential supports for their child and themselves.
Behavioural Therapist
Many children with ASD access behavioural therapy in a group setting or on a one to one basis . Behavioural therapy can help the child to learn more appropriate behaviours and ways to express him/herself and work at decreasing challenging behaviours.
Exercise: Describing Team Members’ Roles
THINK about a child with ASD at your centre.
TRY to generate a list of the various professionals involved in the child’s care of which you are aware.
Describe your understanding of each team member’s discipline and role in the child’s care. Remember that not all information needs to be shared with everyone, so you may not be involved personally with all of the child’s team.
Click here to see a sample answer
How Does the Team Communicate?
It is helpful to have discussed methods of communication with family members before the child enters a child care centre. This ensures that the parents will know how to communicate their concerns to you when they arrive. It also helps parents to know how you will share your observations with them. It may be beneficial to consider keeping a formal record of the communication strategies a family would like to follow.
Program Plans
A program plan is a document designed to facilitate communication among members of a team that formally identifies plans for a child’s program. Different terms are applied to program plans based on the specific goals and objectives of the plan. For example, a child may have a very specific behavioural program plan to teach a particular skill.
This plan might include details such as the following:
- Teaching Objective
- Environment/Setting
- Activity
- Equipment/Material
- Prerequisite Skills
- Teaching Method
- Step 1
- Step 2
- Step 3
- Consequence(s) for correct performance
- Consequence(s) for incorrect performance
- Plan for generalization and maintenance
- Mastery criteria
Although you may develop some specific behaviourally-based program plans, you are likely to also need a plan to cover various components of a child’s program. Routine-based program plans are often developed in conjunction with early interventionists to incorporate teaching strategies into a child’s day-to-day routine. Staff members in early childhood education centres typically develop Individual Program Plans (IPPs) or Individual Education Plans (IEPs) to describe a child’s individualized education, or centre-based program. Increasingly, as intervention teams are developed, there is a focus on the development of Individual Family Service Plans (IFSPs). As part of the IFSP development, the family, centre staff and other team members meet to create a document that focuses on the family and the child’s development across a variety of natural environments.
There are many resources available to assist families and professionals to develop IFSPs and IPP/IEPs (see end of Module). It is recommended that early childhood educators and/or professionals working with children with special needs pursue additional training to gain experience in understanding and developing these important documents. As a guideline, here is a brief outline of the features of an IFSP and an IEP that has been adapted from The Individual Family Service Plan, 2000 and Creating Useful Individualized Education Programs (IEPs), 2000.
Individual Family Service Plan (IFSP)
- Records and guides intervention program
- A written document to facilitate communication among team members
- Includes information about the child’s developmental status (e.g. physical, cognitive, communication, social, and adaptive skills)
- Includes information about the family’s strengths, concerns, priorities, and resources
- Contains a plan to achieve goals/desired outcomes
- Focus on developing particular skills to achieve functional outcomes
- Procedures and timelines are identified
- Service providers and the frequency of service delivery is identified
- Promotes intervention within natural environments
- Identifies a coordinator for contact as well as contact numbers for other people/professionals available for support
- Provides a dynamic document that is regularly reviewed and revised
Individual Education Plan (IEP)/Individual Program Plan (IPP)
- Records and guides education program
- Creates a written document to facilitate communication between the student, family, teachers and other service providers
- Includes information about the child’s current academic performance and may include additional information regarding strengths, weaknesses, behaviour, and school history
- Identifies expectations regarding the child’s learning that are modified from, or alternative to, those of the typical program curriculum
- Will include a transition plan to school and/or other appropriate services
- Contains a plan to achieve the goals and objectives
- Identifies aids, services (service providers and frequency of service delivery) and modifications
- Includes information regarding how communication occurs with parents/family
- Provides a dynamic document that is typically reviewed at least annually
- Includes information regarding transition services
IFSPs and IEP/IPPs have many common features. The IFSP focuses more specifically on the family. The IFSP also has an emphasis on intervention in natural environments. Typically the IFSP has been developed by a team from a variety of settings and therefore facilitates communication among all those involved in a child’s life.
It is important to prepare accordingly when you work with families and facilitate or attend an IPP/IEP or IFSP meeting. The degree of preparation you need will depend upon whether you are facilitating or attending. Some of the following guidelines may be helpful for your preparation, particularly if you are the facilitator:
- Communicate first with the family regarding its preferences for participation, a meeting time, and which individuals to invite.
- Invite all pertinent team members (have a list of names and telephone numbers), using the input from the family.
- Gather relevant documentation and review it prior to the meeting (e.g., reports, work samples).
- Prepare and circulate an agenda
- Arrange seating to facilitate communication.
- Welcome all attendees.
- Identify a “recorder” to take minutes of the meeting and ensure they are distributed to all members afterwards.
- Create a positive environment and encourage each member to express his/her opinions.
- Keep to the schedule (e.g., start and stop on time).
- End on a positive note with documentation of the intervention plan and agreed upon date(s) for follow-up meeting(s).
Regardless of your role you are most likely to have a positive meeting when you are able to participate in an open dialogue, respect and value the input of others.
Communication Books
A communication book helps to promote two-way communication between centre staff, families, and other professionals. A home-school communication book provides an opportunity for parents to share information about a child’s home routine that may affect the child’s behaviour at the centre. For example, if a child has had a short sleep and is likely to be tired the next day you may decrease the expectations placed on the child. A communication book also provides an opportunity for you to learn about significant events the child has experienced. One may use this information to provide activities that cater to the child. For example, if you know the child went to the swimming pool on Saturday, you might notice the child’s splashing gesture (which can be elaborated), or you can talk about how the water feels.
A communication book also helps families know more about what the child does during the day. Children with ASD may have challenges communicating about the day’s events. Short written notes, work samples, and photographs are all helpful ways to communicate. It may be useful to talk to parents to learn which details they would be most interested in learning. It helps to be specific about the events of the day and to share accurate and positive information. For example, rather than reporting that today was a “bad day”, try to say what triggered the behaviour of concern, what the child did exactly, and how it was handled. Then you might report how you are considering managing the situation if it arises another time.
Parent Visits
It is helpful for parents to observe their child interacting with others. Having an “open door” policy so that parents feel welcome to observe their child and the program helps to encourage a collaborative approach. Other professionals may also wish to observe the child in the centre. This may provide the professional with a broader understanding of the child, and create a good opportunity for an on-site consultation about specific issues.
Communicating with the Team to Meet a Challenge
When a child is making progress with their learning objectives, the program plan team may only be periodically involved. When there is cause for concern about changes in behaviour or progress, however, the need for collaboration becomes necessary for all team members.
Members of the child’s team may decide to meet for a number of reasons. For example, they may need to revise a learning objective due to changes in progress or new behaviours. The concern must be clearly stated and communicated among the team members. Be as specific as possible in describing the ABC’s of the situation of concern, or the nature of the child’s difficulty with a particular objective (e.g., Are previous rewards no longer effective? Has the child come to rely on a specific prompt?).
In cases of behaviours you want to reduce/eliminate, use the information from your observations to evaluate the function of the behaviour. That is, carry out a functional analysis (see Module 4). This preliminary information may be invaluable in helping you to define the problem and to decide which team members’ assistance would be beneficial. You may need the parents’ permission to contact other members of the team. Consult your director if in doubt.
Exercise: Choosing a Team Member to Consult
Read the following scenario:
- How would you begin to examine the problem?
- What observations might you make, and what information will you need in order to develop a plan to address the problem?
- What are your initial suggestions for changes?
- If your initial plan does not produce an improvement in the situation within approximately two weeks, whose assistance (e.g., what professionals) might you consult? What would you expect their roles to be?
Click here to see a sample answer
Transition – Preschool to School
Transitions can be challenging for individuals with ASD. Young children and families experience a variety of transitions. The change from a child care setting to school is a significant transition for any child. For those with ASD, a smooth transition may require a higher level of planning. Successful transitions are possible with careful preparation by a committed team of parents and professional partners.
In most jurisdictions, some members of the child’s team (e.g., some health care providers and other professionals) may remain part of the child’s team when they go to school, while others (e.g., early childhood educators) will not, and a new group of providers will become involved (educators and other school-based professionals). Strong transition services prepare families and children for the move, support them during the move, and maintain contact with them to address problems that may arise after the move.
As eligibility for school entry varies across jurisdictions, the child’s parents and child care providers need to be aware of the local eligibility criteria and of the transition process in your school district.
Some school districts have established steps to follow in preparing to support a child with special needs at a school. In other districts, the process could be less formal, or based more on the experience and accessible accommodations of the particular school. Parents often require support to ensure that a plan is in place for their child’s school placement. In some communities, private schools are being established for children with special needs, including ASD. Families may need support as they explore a range of options available to them and their children. During this time there may be periods of uncertainty and additional stress for the family. Preschool educators are often experienced supporters when working with families and children with special needs and can be an asset to a child’s transitional team.
Public and professional awareness of Autism Spectrum Disorder has grown a great deal in recent years. Children diagnosed with ASD vary widely in their skills and their behaviour. The staff of any given school may be unfamiliar with the wide range of abilities and characteristics of children with ASD. Information about the individual needs of the child you are working with must determine the services provided to him/her.
It is beneficial when families provide documentation about the child’s special needs in the form of reports from professionals who have assessed them or provided intervention services (e.g., speech-language pathologist, psychologist).
Usually a transition meeting will be held in the spring prior to the child beginning school. This meeting brings together parents, preschool educators, other consultants (e.g., speech-language pathologist, occupational therapist, psychologist), and those who will be contributing to the school-based program (e.g., principal, classroom teacher, resource teacher, speech-language pathologist). The goal of this initial transition meeting should be to devise a plan to introduce the child to the school, and vice versa, in as systematic a way as possible. Other meetings will be required to develop the school-based IPP (or IEP: Individual Education Plan or Program), which is often an outgrowth of the preschool IFSP.
The child’s parents may share written reports in advance of this conference, where the focus will be on facilitating a smooth transition from preschool to school. Information from the preschool program will include a description of the setting and routines, as well as the child’s individual program plan and records of his/her accomplishments. Preschool educators have the important role of sharing their knowledge about and experience with the child in a group setting. This information is crucial in ensuring a successful transition into school. Decisions such as the type and amount of support (e.g., dedicated time from an educational program assistant) may depend on a detailed analysis of the child’s ability to learn and interact within peer groups.
Remember, successful transitions are characterized by:
- Children’s positive attitudes
- Parents’ positive attitudes
- Teacher’s provision of developmentally-appropriate experiences
- Communities that provide support – sharing, cooperating, and coordinating across agencies
Try to be mindful of the differences in how preschool and school systems operate with respect to the number of children, types of learning environments (including physical spaces) and the different administrative structures and range of professionals involved. While information from the child care setting is valuable, one cannot entirely predict how a child with ASD will adapt to the demands of the school setting, based only on their preschool experiences.
Review
Families of children with ASD usually require many professionals to support the needs of their child and the family, but ultimately the goal is to meet the family’s needs. The collaborative efforts of team members should be directed toward empowering the family and helping to ensure that the child’s care and education match his/her needs. Good communication is a key to effective collaboration. When major transitions take place, special care must be taken to ensure that appropriate information is passed along at the right time, and in the most helpful way. Early childhood educators play a key role in providing observations of the child in a group setting, and in reporting the effectiveness of specific intervention strategies for the individual child.
Enabling Person-Directed Planning for Augmentative and Alternative Communication (AAC) Users
The Enabling Person-Directed Planning for AAC Users guidebook, is designed to help persons who use augmentative and alternative communication take an active role in the person-directed planning process. The guidebook outlines a 5-phase process, based on established best-practices in AAC and transition planning for persons with disabilities, for developing partner communication strategies with planning recipients who use AAC.
Enabling Person-Directed Planning for AAC Users: Guidebook
Once you have read through the guidebook, you can download the specific toolkits (sample checklists) and blank templates that are included within the guide for use later.
Screening Tools for Information on AAC Usage
Gathering Preliminary AAC Information/Current AAC Usage
Communication Context Interview / Observation
AAC Considerations Matrix for Person-Directed Planning
Social Skills Matching Game
- The game can be played with 2-4 players.
- Place the cards face down in the middle of the players.
- Each player has a turn and picks up a card. The player turns the card over and acts out the activity shown on the card. (For example, if the card is hello, the child waves or says “hi “to the other players). An adult may need to help the child act out the activity.
- Then the player places the card on the matching square contained on his/her board.
- The game is over when all the players have the matching pieces on their boards.
- If a player turns over a card she/he already has:i.e. bubbles, she/he gives the card to a friend who does not have the card yet. The friend acts out the activity:i.e. blows bubbles and then, the player who shared the card is given another turn to find a new card.
Activities for each card:
- Card one: Say “hi” to your friend
- Card two: Shake hands with your friend (or the whole group)
- Card three: Blow bubbles to a friend
- Card four: Give a friend a high five (or the whole group)
- Card five: Hug
- Card six: Sing a song with your friends. The child who has the card can choose the song and everyone sings. Possible songs include: Row Row Your Boat, Ring Around the Rosie, etc.
*To facilitate socialization, it is important that an adult be involved in the game and assist
*An example of possible activity pictures depicting the activities for the matching board and cards is on page two of this document. You can create the matching board and cards using drawn pictures, magazine pictures or photographs.
Example of Pictures for Social Game Board and Cards.
(taken from the Boardmaker Program:Mayer-Johnson Co.)