Print out and use

An interactive presentation on Person Directed Planning tools and resources.

There are many transitions in life. This Guide focuses on the transition to older adulthood for people with developmental disabilities. It is important to keep in mind that transition to older adulthood is not merely about accessing a variety of programs available to senior citizens. It is above all a planned and conscious evolution to embrace life as it presents itself during the aging process.
From the Ontario Partnership on Aging and Developmental Disabilities
A Bi-monthly Newsletter of The Toronto Partnership on Aging and Developmental Disabilities (TPADD)
The Advocacy Centre for the Elderly (ACE) is a specialty community legal clinic that was established to provide a range of legal services to low-income seniors in Ontario. The legal services include advice and representation to individual and group clients, public legal education, law reform and community development activities. ACE has been operating since 1984.
ACE Brochure: Click here
ACE website: Click here
Angela Gonzales and Lindsay Wingham-Smith discuss ways to improve collaborative care planning to support people with issues related to aging with a Developmental disability Click here
A BRAND NEW WORLD: ONTARIO’S NEW LONG-TERM CARE HOMES ACT
The Long-Term Care Homes Act, 2007 (LTCHA or the Act) is coming into force in Ontario on July 1, 2010. This legislation replaces the three current pieces of legislation which presently govern long-term care homes: the Charitable Homes Act, the Homes for the Aged and Rest Homes Act and the Nursing Homes Act.
Click here
DISCHARGE FROM HOSPITAL TO LONG-TERM CARE: ISSUES IN ONTARIO
Hospitals in Ontario are overcrowded. Thousands of people are on waiting lists for long-term care homes. As a result, people requiring long-term care (LTC) are confronted with a variety of “policies” and “programs” developed to “deal” with these issues despite the legislation governing placement.
Click here
TIPS AND TRAPS WHEN CONSIDERING APPLYING FOR LONG-TERM CARE
ACE often provides advice regarding issues related to placement or waiting for placement into long-term care. The following are tips and traps that we believe everyone should be aware of when considering long-term care placement or alternatives.
Click here
Long-Term Care: Reframing the Conversation
HOME FIRST” – IS IT RIGHT FOR YOU?
Recent articles have appeared in various publications touting “Home First” programs as the solution to the problem that Alternate Level of Care (ALC) patients face in many hospitals. ALC patients have completed the acute phase of their treatment and are awaiting placement into a long-term care home, but because of long waiting lists remain in hospital. While “Home First” may be beneficial for many seniors, this is not universal.
Click here

Professional Fatigue: Surviving the Front Lines!
Shared Learning presentation
Presented by: Angie Gonzales, RN MN Health Care Facilitator, Toronto Network of Specialized Care, Surrey Place Centre
Play – For tablets (HTML 5)
Professional Fatigue: Surviving the Front Lines!
Shared Learning presentation
Presented by: Sue Hutton, Community Living Toronto
Play – For tablets (HTML 5)
Becoming Present Exactly As We Are
5 Touchstone Techniques
Related PDFs

Advice in the areas of wills, trusts and estate planning for individuals with disabilities and their families.
Recorded on Monday, October 20, 2014 at the Victoria Village Hub 1527 Victoria Park Ave., 2nd Floor 7:00 – 9:00 pm
The Advocacy Centre for the Elderly (ACE) is a specialty community legal clinic that was established to provide a range of legal services to low-income seniors in Ontario. The legal services include advice and representation to individual and group clients, public legal education, law reform and community development activities. ACE has been operating since 1984.
ACE Brochure: Click here
ACE website: Click here
A BRAND NEW WORLD: ONTARIO’S NEW LONG-TERM CARE HOMES ACT
The Long-Term Care Homes Act, 2007 (LTCHA or the Act) is coming into force in Ontario on July 1, 2010. This legislation replaces the three current pieces of legislation which presently govern long-term care homes: the Charitable Homes Act, the Homes for the Aged and Rest Homes Act and the Nursing Homes Act.
Click here
DISCHARGE FROM HOSPITAL TO LONG-TERM CARE: ISSUES IN ONTARIO
Hospitals in Ontario are overcrowded. Thousands of people are on waiting lists for long-term care homes. As a result, people requiring long-term care (LTC) are confronted with a variety of “policies” and “programs” developed to “deal” with these issues despite the legislation governing placement.
Click here
TIPS AND TRAPS WHEN CONSIDERING APPLYING FOR LONG-TERM CARE
ACE often provides advice regarding issues related to placement or waiting for placement into long-term care. The following are tips and traps that we believe everyone should be aware of when considering long-term care placement or alternatives.
Click here
HOME FIRST” – IS IT RIGHT FOR YOU?
Recent articles have appeared in various publications touting “Home First” programs as the solution to the problem that Alternate Level of Care (ALC) patients face in many hospitals. ALC patients have completed the acute phase of their treatment and are awaiting placement into a long-term care home, but because of long waiting lists remain in hospital. While “Home First” may be beneficial for many seniors, this is not universal.
Click here

Aging with A Developmental Disability – Lifestyle & Health Considerations
Tip sheets and workshop describing the likely changes to their body systems and functioning abilities as someone ages and strategies to help support a person with an intellectual disability exhibiting these changes.
Original material compiled by Jane Powell of L’Arche Ontario. Adapted with permission from http://www.aging-and-disability.org
Presenter: Brenda Elias, Faculty, Non Profit and Voluntary Sector Management, Ryerson University and Social Foundations of Gerontology, Family & Community Social Services, University of Guelph-Humber
Critical importance of social networks for maintaining health and wellbeing as we age
Centennial College Nursing Students Presentation Series 2012: Sensory changes that occur with the elderly and strategies to overcome the impacts
Presenter: Susan Hui
Some of the common concerns around nutrition and eating as they relate to aging and some strategies that can be used to help maintain the nutritional level of those we support.
Centennial College Nursing Students Presentation Series 2012: Fall prevention risk assessments and strategies to prevent falls and fall injuries.
The focus of this article is about maintaining foot health and the caregiver’s role in preventing foot complications. Read more
Palliative care can be separated into three stages. These stages enable the caregiver to plan and work with expected outcomes. In each of these stages symptom management is required, the following pages cover the most common symptoms. Material written by Aakilah Ade, Certified Hospice and Palliative Care Consultant.
Palliative Care and Symptom Management
Good health is important to all of us. When you are healthy, you can go out with friends and family, do sports, go to school, or work better. People with developmental disabilities are more likely to have illnesses like diabetes, asthma or heart disease than people without a disability.
This video explains how healthy people with developmental disabilities in Ontario are, and what kind of healthcare they get. Not everyone is as healthy as they could be, and not everyone is getting the healthcare that they need.
Caption: A Talk About Health, by Health Care Access Research and Developmental Disabilities (H-CARDD), CAMH, 2015 [20 minutes]
The more the doctor knows about you, the more they can help make the visit better for you. Use the “About My Health” form to write down information about you, your medication, and your health before you go see the doctor. You can fill it out yourself or ask someone to help you. Give this form to your doctor or nurse at the start of any healthcare visit. Get the “About My Health” form at the Surrey Place website.
Sometimes it is difficult to remember everything that the doctor said. Ask your doctor or someone who comes with you to the doctor’s office to fill out the “About My Healthcare Visit” form. Write what you need to do after the healthcare visit. Get the “About My Healthcare Visit” form at the Surrey Place website.
Even if you don’t feel sick, it is still important to see your doctor once every year for a check-up. In this video Andrew explains what happens at a healthcare visit and how you can prepare.
Caption: Going to the Doctor, by Health Care Assess Research and Developmental Disabilities (H-CARDD), CAMH, 2016 [5:30 minutes]
Sometimes the doctor needs to know more about your health and will ask you to get a blood test at a health lab. This video shows you what exactly happens when going for a blood test.
What happens when you go to get bloodwork done, by Surrey Place, 2019, [3:00 minutes
Getting a Blood Test, by Health Care Access Research and Developmental Disabilities (H-CARDD), CAMH, 2016 [4:30 minutes]
When you go to the hospital or emergency room, people will ask you many questions. Bring the “About My Health” form to have all your information ready for the doctors and nurses.
This video explains what happens when you go to the emergency department.
Caption: What to expert wen you go to the ER, by CAMH, 2014 [3:10 minutes]
Find more tips on how to prepare for a visit to the emergency department in this checklist.
Prepare a crisis plan with your family or staff for future emergencies.
Sometimes you don’t notice when you are sick. At a check-up you can ask for tests to see if you are healthy. Some important health problems to check for are: cancer, diabetes, pap test. Here are some other things to know about health.
Mental health is about how you feel and what you think. Sometimes you do not feel sick in your body, but you just don’t feel happy or enjoy doing activities anymore, or you worry a lot. Listen to a conversation with Special Olympics athletes about what you can do when you don’t feel happy and how you can help others who feel that way. There are 4 videos in this series.
A Conversation About Mental Health with Special Olympics Athletes, by H-CARDD and Special Olympics, 2016
We all like to have someone in our corner in difficult situations. Staff can make a big difference in supporting people with developmental disabilities in their health. Learn how to prepare together for a visit to the doctor.
Caption: Everybody Wins: Preparing for a Healthcare Visit. By, Health Care Access Research and Developmental Disabilities and Vita Community Living, 2019 [7:06 minutes]
During the healthcare visit support workers can help with communication. In this video you see how to use the About My Health and My Healthcare Visit forms to share important information with the doctor. Julie also shares how a few accommodations can really be a game changer for her healthcare visit.
Caption: The Game Changer: The Doctor Visit, by Health Care Access Research and Developmental Disabilities and Vita Community Living, 2019 [7:55 minutes]
Support staff can also help track common health issues like bowel movements, sleep and weight using monitoring charts. Download health monitoring charts.
For a complete healthcare toolkit for direct support professionals, visit the website Nuts and Bolts of Health Care. The toolkit includes, videos, tools and newsletters with practical tips on primary and emergency care.
Community Networks of Specialized Care (CNSC): this network links specialized services across Ontario, improves services delivery and builds capacity in the community. The team includes Health Care Facilitators across Ontario. This website has information for service providers and direct support professionals Read more.
Developmental Disabilities Primary Care Program (DDPCP): this program develops guidelines, resources and tools for health care providers and caregivers to improve the health of people with developmental disabilities. Read more.
Health Care Access Research and Developmental Disabilities (H-CARDD): this is a research program investigating the health status and health service use of adults with intellectual and developmental disabilities in Ontario. On this website you will find research information and many clinical tools and health care resources for patients, caregivers, and health care providers. Read more.
Presenter: Tracey Human, RN, Palliative Pain Symptom Management Consultation Service for Toronto
Considerations for intellectual and physical disability communities of practice – palliative care, hospice, collaborative care planning.
Professional Fatigue: Surviving the Front Lines (Shared Learning Forum November 2013)
Presented by: Angie Gonzales, RN MN Health Care Facilitator, Toronto Network of Specialized Care, Surrey Place Centre
Professional Fatigue: Surviving the Front Lines (Shared Learning Forum November 2013)
Presented by: Sue Hutton, Community Living Toronto
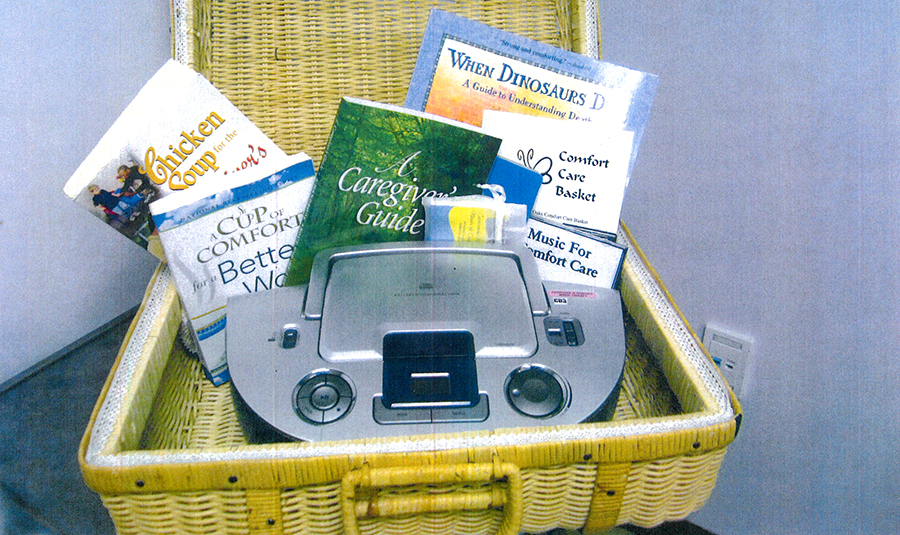
Comfort Care is an essential part of medical care at the end of life. It is care that helps or soothes a person who is dying. The goal is to prevent or relieve suffering as much as possible while respecting the dying person’s wishes. Seven Oaks Long Term Care Home has developed a Comfort Care Basket program. The Comfort Care Basket is for the resident who is currently receiving comfort care support, their family and friends in hope that it will make their time together as comfortable as possible. This guide details how to create a Comfort Care Basket, ideas about what you can do to provide comfort care and specific protocols for various cultural and religious beliefs. Read more »
Death comes differently for every person, and your loved ones death will be unique. However, there are changes that are commonly part of this final phase of life. You may see these in your loved one. This handout explains some of these changes and gives ideas about what you can do to provide care and comfort. This information may help you anticipate the changes you may see in your loved one and to go forward with more peace and confidence. Read more »
A glossary of palliative and end of life terms and definitions Read more »
Living in a society represented by many cultures and religious beliefs means that memorable events can be celebrated differently. In this section we look at the different religious beliefs surrounding death & dying and what funeral or burial rituals may be undertaken. Read more »
The My Health Booklets are a series of health education booklets produced by Surrey Place Centre and funded by the Ontario Government, Ministry of Children, Community and Social Services. The purpose for the series is to offer guidance to people with developmental disabilities in a clear and simple manner. The series consists of eight booklets now available online, with subjects ranging from general health issues to more specific health topics.
Jillian Carlyle of the CAMH Dual Diagnosis Service talks about what clients and families should expect and prepare for when going the emergency department. Play video
This article offers some practical tips about how to make emergency visits as good as they can be, and also outlines some steps we can all take to reduce the likelihood of having to go to the hospital in the first place. read more
Useful strategies to improve communications and gather more comprehensive information on people with developmental disabilities who come to medical settings requiring medical support.
After the presentation Kim gives a description about her role as a care coordinator for client’s that receive services/supports through TC LHIN and how this intersects with the developmental sector services/supports. Play video
The waiting room can be a very difficult and often chaotic environment for anyone. Below are some helpful tips and tricks to help win the waiting game. It is important to remember that the way one can support a person during a doctor’s visit will depend on their individual needs and preferences. Read more
Being regular, particularly in adulthood, is an “irregular” conversation starter. It is one of those topics that seem too “private” or perhaps too “stinky” to discuss in public. But the reality is that how we feel each day is closely tied to our bowels. Read more
Women with developmental disabilities are less likely than other women in Ontario to have a pap smear which is how doctors screen for cervical cancer. They are also less likely to get a mammogram to detect breast cancer. Why does this matter? If we have health problems and they aren’t detected early, small problems can become big ones, and can even lead to death. Every woman has a right to get health care early before problems become too serious. Read more
While men in general can have health problems that they often ignore because they don’t like to talk about their health and how they are feeling, having a disability makes it even harder. Read more
Medication use is very common for individuals with developmental disabilities. But medications can also lead to problems when you struggle with how to report whether a medication helps or not, or when others aren’t alert to the impact of the side effects. Read more
When considering the issue of quality of life for people with developmental disabilities, and particularly with those who have challenging behaviour, it is important to consider the role of sensory engagement in a holistic biopsychosocial approach. Read more
Let’s Talk: An Open Dialogue on Vulnerability in Toronto Series:
Through collaboration and coordination, the Community Network of Specialized Care works to build efficient and effective cross-sectorial specialized service systems that support people with a developmental disability and mental health challenges (dual diagnosis) and/or challenging behaviour. Read more
Presenting preliminary findings on ACT’s “ASD & HIV Prevention Needs Assessment” survey and explaining the impact the autism spectrum has on negotiating safer sex, accessing services, and community connection. Play video
The purpose of the Community Networks of Specialized Care is to enhance service to adults with a developmental disability who need specialized care for co-existing mental health and or/ behavioural issues in Ontario. There are 4 networks: Northern Region, Southern Region, Eastern Region and Central Region. http://www.community-networks.ca
Excerpt from “Neurodevelopmental Disabilities” (Let’s Talk: An Open Dialogue on Vulnerability in Toronto Series)
Presenter: Lisa Orsi, Centre for Addiction and Mental Health (CAMH)
Excerpt from “Neurodevelopmental Disabilities” (Let’s Talk: An Open Dialogue on Vulnerability in Toronto Series)
Presenters: Angie Gonzales and Aamir Khan, Community Network of Specialized Care.
The Developmental Disabilities Primary Care Initiative has brought together clinicians with expertise in the care of adults with developmental disabilities (DD) to improve primary care and quality of life for adults with developmental disabilities (DD). Primary Health Care of Adults with Developmental Disabilities Guidelines
With leadership and coordination from Surrey Place Centre, and funding from the Ontario Ministry of Children, Community and Social Services, the Ontario Ministry of Health and Long-Term Care, and Surrey Place Centre Foundation, Guidelines and Tools have been developed to help primary care providers to follow best practices in the care of these patients. These guidelines and tools are utilized in the Training Course for primary care providers that are offered on a yearly basis.
Health and longevity is related to lifestyle and predisposition to certain health conditions. Aging well depends on maintaining one’s health by making healthy choices. This checklist can help to identify aspects of the individual’s lifestyle that may result in health problems and those that promote good health. After completing the checklist, a good next step is to develop a plan for helping the person adjust their lifestyle choices wherever possible.
Do the person’s eating habits reflect awareness of and adherence to the Canada Food Guide? (For more information on the Canada Food Guide go to https://food-guide.canada.ca/en/
If not, what areas need to be changed?
What is the person’s weight and height? Is this a concern? How does it compare to the norm?
What does the person do for exercise? Is it done regularly? If not what are the possible physical activities the person may wish to start?
What are the risk factors associated with his/her place of residence?
Name / Dosage / Purpose
Sourced from “Transition Guide For Caregivers”, The Ontario Partnership on Aging and Developmental Disabilities http://www.opadd.on.ca
There is evidence that men and women with developmental disabilities are subject to some differences in the onset and progress of aging due to hereditary, environmental and lifestyle factors. This adds to the complexity of the aging process for this population and increases the challenge facing caregivers.
While many people with a developmental disability enjoy the same life expectancy as the general population, there is evidence that the effects of aging can begin earlier and progress more quickly in some cases. Consequently, while all people begin to experience the effects of aging in their 40’s, some persons with a developmental disability may require a greater level of adjustment in support at a younger age than the general population. Caregivers must pay attention to factors associated with aging such as changes in social roles, activity level, interests, behaviour patterns, response to things in the environment and health conditions, if they are to provide effective support.
Some of the genetic aspects of specific developmental disabilities may impact the aging process. For example, persons with Down Syndrome are subject to a number of factors that can influence the onset and progression of aging. These include:
People with Prader-Willi syndrome are at higher risk of diabetes mellitus. Diabetes results in the debilitation of internal organs and can result in severe compromises to health and even death.
Central nervous system compromise resulting in an associated developmental disability such as epilepsy, cerebral palsy and some forms of visual impairment may exacerbate the onset and progression of aging.
Where a person lives may influence health and result in conditions that affect the aging process. For example, institutional settings may pose risks of infections; community group home settings may pose risk due to lifestyle choices that result in lack of exercise, smoking, alcohol consumption, poor diet, unsafe sex, drug use.
Access is not merely about getting an appointment with a physician or visiting a clinic. People with developmental disabilities often have health problems associated with their developmental disability. For this reason it is important that the health care practitioner, who may not have much knowledge of developmental disabilities, receives guidance on a monitoring regime that fits with the needs and risks of the individual. It is also important to find the right practitioners with the requisite specialties that are needed by the individual.
Persons with a developmental disability may not always have insight into the effect that aging is having on them. They may be unable to articulate what they are experiencing in ways that other people understand what they are experiencing. Consequently there is the potential for signs of aging to go unnoticed until they become more pronounced. Caregivers should consider how to inform and educate people with developmental disabilities about aging and the ways in which they may choose to adjust their lifestyle to accommodate older adulthood. Caregivers must also educate themselves about aging issues so they are prepared to monitor and to intervene with age-related needs. Finally, caregivers who know the person well should be sure to educate others in the support circle and caregivers in new services which the person may access, about the communication style of the individual and some of the key messages that they generally communicate to others.
The aging of persons with a developmental disability may occur at a younger age than the general population and be affected by factors related to their specific disability. It is important that caregivers pay attention to the indicators of aging such as changes in social roles, activity level, interests, behaviour patterns, response to things in the environment and health conditions. More information about specific developmental disabilities and their potential effects on aging can be obtained from your physician, local library and Internet sites.
Have you noticed any changes in the person over the past year?
If YES, what kinds of changes?
Sourced from “Transition Guide For Caregivers”, The Ontario Partnership on Aging and Developmental Disabilities http://www.opadd.on.ca
One of the important things that can make a difference to remaining in one’s own home may be the accessibility features of the residence. If a person experiences lessened mobility, stairs may pose a challenge. A person with symptoms of dementia may wander away from the home resulting in the need for electronic systems to monitor their whereabouts. It is important to consider the various accessibility features of the home and the potential of retrofitting to add new features. Some homes may lend themselves to such changes and some may not. Knowing what the potential is for the person’s present home can help to plan ahead for remaining at home or moving if certain circumstances present themselves.
Sourced from “Transition Guide For Caregivers”, The Ontario Partnership on Aging and Developmental Disabilities http://www.opadd.on.ca